Acute Coronary Syndrome (ACS) is a term used to describe a range of medical conditions associated with sudden loss of blood flow to the heart. One of the most common forms of ACS is the Acute Coronary Condition, often abbreviated as ACC. It's crucial to understand that ACC is not a diagnosis in itself but rather a symptom complex that can lead to various diagnoses, including myocardial infarction (heart attack) and unstable angina. The term "ACC" has been used variably in medical literature and practice, sometimes causing confusion among healthcare professionals and patients alike.
Understanding the nuances of ACC requires delving into the pathophysiology of coronary artery disease. The coronary arteries supply blood to the heart muscle, and any condition that reduces blood flow through these arteries can lead to ischemia (reduced oxygen delivery) or infarction (death of heart tissue due to lack of oxygen). Conditions like atherosclerosis, where plaque builds up in the arteries, can lead to narrowing or blockage of these critical vessels. The clinical presentation of ACC can vary widely, from chest pain (angina) that occurs at rest or with minimal exertion, to more severe forms like non-ST-elevation myocardial infarction (NSTEMI) or ST-elevation myocardial infarction (STEMI), which are types of heart attacks.
Key Points
- Acute Coronary Condition (ACC) refers to a range of symptoms associated with reduced blood flow to the heart.
- ACC is not a specific diagnosis but can lead to diagnoses like myocardial infarction or unstable angina.
- The pathophysiology involves conditions that reduce blood flow through the coronary arteries, such as atherosclerosis.
- Clinical presentations vary from angina to severe forms like NSTEMI or STEMI.
- Timely and accurate diagnosis is critical for appropriate management and outcomes.
Diagnosis and Management of ACC
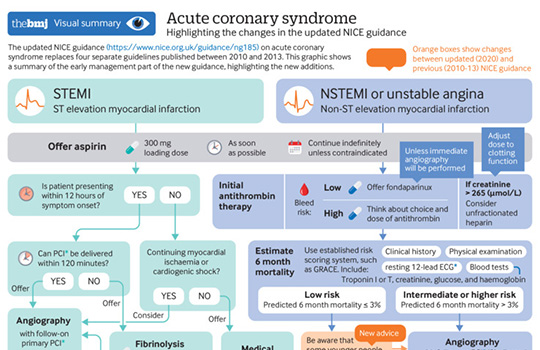
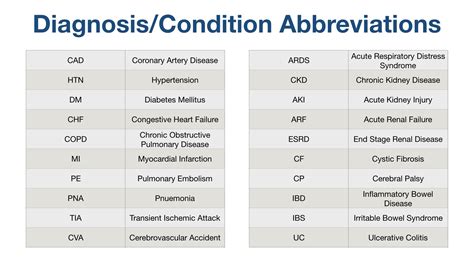
Diagnosing the underlying cause of ACC involves a combination of clinical assessment, electrocardiogram (ECG), blood tests for biomarkers like troponin, and imaging studies such as echocardiography or coronary angiography. The management strategy depends on the specific diagnosis but generally involves immediate medical therapy to restore blood flow, reduce the heart’s workload, and prevent further clotting. For example, in the case of a heart attack, prompt administration of thrombolytic therapy or primary percutaneous coronary intervention (PCI) is crucial to salvage the affected heart muscle.
Role of Medical History and Risk Factors
A thorough medical history and identification of risk factors are essential in the evaluation of patients with suspected ACC. Risk factors for coronary artery disease, such as hypertension, diabetes mellitus, hyperlipidemia, smoking, and family history of heart disease, can guide the clinician in assessing the likelihood of an acute coronary event. Additionally, understanding the patient’s symptoms, including the nature, severity, and duration of chest pain, can provide valuable insights into the potential diagnosis and appropriate management strategy.
| Risk Factor | Relevance to ACC |
|---|---|
| Hypertension | Increases the risk of coronary artery disease and subsequent ACC |
| Diabetes Mellitus | Enhances the risk of atherosclerosis and worsens outcomes in ACC |
| Hyperlipidemia | Contributes to the development of atherosclerotic plaques in coronary arteries |
| Smoking | A significant risk factor for coronary artery disease and ACC |
| Family History | Increases the risk of premature coronary artery disease |

Prevention and Long-term Management

Preventing the development of coronary artery disease and reducing the risk of ACC involves lifestyle modifications and, when necessary, medical therapy. Lifestyle changes include adopting a healthy diet, engaging in regular physical activity, smoking cessation, and maintaining a healthy weight. For patients with established coronary artery disease, long-term management focuses on secondary prevention, including the use of antiplatelet agents, statins to manage cholesterol, beta-blockers to reduce the heart’s workload, and, in some cases, coronary artery bypass grafting (CABG) or PCI to restore blood flow.
Emerging Trends and Technologies
The field of cardiology is rapidly evolving, with emerging trends and technologies offering new hope for the diagnosis, management, and prevention of ACC. Advances in imaging techniques, such as coronary computed tomography angiography (CCTA), and the development of novel biomarkers are improving diagnostic accuracy. Moreover, innovations in percutaneous interventions, including the use of bioresorbable vascular scaffolds, and advancements in pharmacotherapy, such as the introduction of PCSK9 inhibitors for lipid management, are expanding treatment options for patients with coronary artery disease.
What are the common symptoms of Acute Coronary Condition (ACC)?
+Chest pain or discomfort, shortness of breath, nausea, and fatigue are common symptoms. However, some individuals, especially women and those with diabetes, may experience atypical symptoms.
How is ACC diagnosed?
+Diagnosis involves clinical assessment, ECG, blood tests for troponin and other biomarkers, and imaging studies like echocardiography or coronary angiography.
What are the management options for ACC?
+Management depends on the specific diagnosis but includes medical therapy to restore blood flow, reduce heart workload, and prevent clotting, as well as interventions like PCI or CABG in selected cases.
In conclusion, ACC represents a spectrum of acute coronary conditions that require prompt recognition and management to improve patient outcomes. Through a combination of lifestyle modifications, medical therapy, and when necessary, invasive interventions, it is possible to reduce the risk and impact of these conditions. As research and technology continue to evolve, the future of cardiology holds promise for even more effective strategies in the prevention and management of coronary artery disease and its acute manifestations.