The concept of acute medication definition is multifaceted and plays a crucial role in the management of various medical conditions. At its core, acute medication refers to the pharmacological treatment of acute illnesses or injuries, which are typically characterized by a rapid onset and a relatively short duration. These conditions can range from common ailments such as acute bronchitis, pneumonia, and urinary tract infections to more severe emergencies like myocardial infarction (heart attack) and stroke. The primary goal of acute medication is to alleviate symptoms, prevent complications, and facilitate recovery in the shortest possible time frame.
Acute medications are often distinguished from chronic medications, which are used to manage long-term conditions such as diabetes, hypertension, and arthritis. While chronic medications are typically taken over an extended period, sometimes for the rest of a patient's life, acute medications are prescribed for a limited duration, usually until the acute condition resolves or significantly improves. The selection of acute medication depends on the specific condition being treated, the severity of symptoms, the patient's medical history, and potential interactions with other medications the patient may be taking.
Key Points
- Acute medication is used to treat acute illnesses or injuries with a rapid onset and relatively short duration.
- The primary goal of acute medication is to alleviate symptoms, prevent complications, and facilitate recovery.
- Acute medications are distinguished from chronic medications by their limited duration of use.
- The selection of acute medication depends on the specific condition, symptom severity, patient history, and potential drug interactions.
- Examples of acute conditions include acute bronchitis, pneumonia, urinary tract infections, myocardial infarction, and stroke.
Pharmacological Principles of Acute Medication
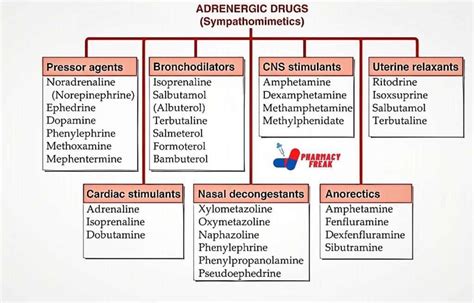
The pharmacological management of acute conditions involves a deep understanding of the underlying pathophysiology of the disease, the mechanism of action of the medication, and the pharmacokinetics and pharmacodynamics of the drug. Pharmacokinetics refers to how the drug is absorbed, distributed, metabolized, and excreted by the body, while pharmacodynamics concerns the effects of the drug on the body. For instance, in the treatment of acute bacterial infections, antibiotics are chosen based on their spectrum of activity, the site of infection, and the patient’s ability to tolerate the drug.
Antibiotics as Acute Medications
Antibiotics are a prime example of acute medications, used to treat bacterial infections. The choice of antibiotic depends on the type of bacteria causing the infection, as different antibiotics have different spectrums of activity. For example, penicillin is effective against streptococcal infections but may not be effective against staphylococcal infections, which might require drugs like methicillin or vancomycin. The inappropriate use of antibiotics, such as using them to treat viral infections, can lead to antibiotic resistance, making these drugs less effective against future bacterial infections.
| Condition | Common Acute Medications |
|---|---|
| Acute Bronchitis | Antibiotics (if bacterial), bronchodilators, cough suppressants |
| Urinary Tract Infections | Antibiotics (e.g., trimethoprim/sulfamethoxazole, ciprofloxacin) |
| Myocardial Infarction | Aspirin, beta blockers, ACE inhibitors, thrombolytics |

Challenges and Considerations in Acute Medication Management

Despite the advancements in pharmacotherapy, the management of acute conditions with medication poses several challenges. One of the significant concerns is the potential for adverse drug reactions (ADRs), which can range from mild to severe. The risk of ADRs is heightened in certain populations, such as the elderly and those with renal or hepatic impairment, due to altered drug metabolism and excretion. Additionally, the emergence of antibiotic-resistant bacteria and the inappropriate use of medications can complicate the treatment of acute infections.
Another challenge is ensuring patient adherence to the prescribed medication regimen, especially in cases where the treatment duration is short, and the patient may feel better before completing the full course of therapy. Patient education plays a critical role in addressing these challenges, as informed patients are more likely to understand the importance of their medication, potential side effects, and the need to complete the prescribed treatment course.
Future Directions in Acute Medication
The future of acute medication management is likely to be influenced by several factors, including advances in pharmacogenomics, which allows for tailored therapy based on an individual’s genetic makeup, and the development of new antimicrobial agents to combat resistant pathogens. Moreover, the integration of technology, such as mobile health applications and electronic health records, can enhance patient engagement, improve adherence, and facilitate more efficient communication between healthcare providers.
What is the primary goal of acute medication?
+The primary goal of acute medication is to alleviate symptoms, prevent complications, and facilitate recovery in the shortest possible time frame.
How does the choice of antibiotic depend on the type of bacterial infection?
+The choice of antibiotic depends on the type of bacteria causing the infection, as different antibiotics have different spectrums of activity. For example, penicillin is effective against streptococcal infections but may not be effective against staphylococcal infections.
What are some challenges in the management of acute conditions with medication?
+Challenges include the potential for adverse drug reactions, the risk of antibiotic resistance, ensuring patient adherence to the prescribed medication regimen, and the need for continuous patient education.
In conclusion, the definition and management of acute medication are complex and multifaceted, requiring a deep understanding of pharmacological principles, disease pathophysiology, and patient-specific factors. As healthcare continues to evolve, the rational use of acute medications will remain a cornerstone of effective patient care, necessitating ongoing education, research, and innovation to address emerging challenges and improve outcomes.