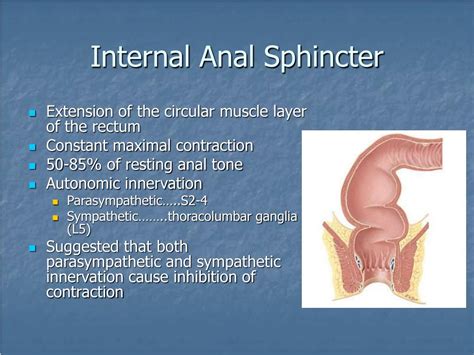
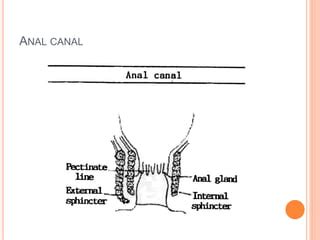
The anal sphincter muscles play a crucial role in maintaining fecal continence and enabling the controlled passage of stool from the body. These muscles are located in the anal canal and are composed of two main types: the internal anal sphincter (IAS) and the external anal sphincter (EAS). The IAS is a smooth muscle layer that is involuntary, meaning it is not under conscious control, while the EAS is a striated muscle layer that is voluntary, allowing for conscious control over defecation.
The anatomy of the anal sphincter muscles is complex, with the IAS being a thick, circular layer of smooth muscle that surrounds the anal canal. This muscle layer is responsible for maintaining a constant resting tone, which helps to keep the anal canal closed and prevent involuntary loss of stool. The EAS, on the other hand, is a thinner, circular layer of striated muscle that surrounds the IAS. This muscle layer is responsible for voluntary contractions, which help to further tighten the anal canal and prevent stool passage.
Key Points
- The anal sphincter muscles are composed of two main types: the internal anal sphincter (IAS) and the external anal sphincter (EAS)
- The IAS is a smooth muscle layer that is involuntary, while the EAS is a striated muscle layer that is voluntary
- The anal sphincter muscles play a crucial role in maintaining fecal continence and enabling the controlled passage of stool from the body
- Dysfunction of the anal sphincter muscles can lead to fecal incontinence, a condition characterized by involuntary loss of stool
- Treatment options for anal sphincter muscle dysfunction include pelvic floor physical therapy, biofeedback, and surgery
Function of the Anal Sphincter Muscles
The anal sphincter muscles work together to maintain fecal continence and enable the controlled passage of stool from the body. The IAS is responsible for maintaining a constant resting tone, which helps to keep the anal canal closed and prevent involuntary loss of stool. The EAS, on the other hand, is responsible for voluntary contractions, which help to further tighten the anal canal and prevent stool passage. When the rectum is filled with stool, the IAS relaxes, allowing the stool to enter the anal canal. The EAS then contracts, helping to expel the stool from the body.
Types of Anal Sphincter Muscle Dysfunction
There are several types of anal sphincter muscle dysfunction, including fecal incontinence, anal fissures, and anal fistulas. Fecal incontinence is a condition characterized by involuntary loss of stool, and can be caused by weakness or damage to the anal sphincter muscles. Anal fissures are small tears in the lining of the anal canal, and can cause pain and bleeding during defecation. Anal fistulas are abnormal connections between the anal canal and the skin, and can cause chronic infection and drainage.
| Condition | Description |
|---|---|
| Fecal Incontinence | Involuntary loss of stool due to weakness or damage to the anal sphincter muscles |
| Anal Fissures | Small tears in the lining of the anal canal, causing pain and bleeding during defecation |
| Anal Fistulas | Abnormal connections between the anal canal and the skin, causing chronic infection and drainage |
Treatment Options for Anal Sphincter Muscle Dysfunction
Treatment options for anal sphincter muscle dysfunction depend on the underlying cause and severity of the condition. Pelvic floor physical therapy, biofeedback, and surgery are all potential treatment options. Pelvic floor physical therapy involves exercises and techniques to strengthen the anal sphincter muscles and improve their function. Biofeedback involves the use of specialized equipment to help patients become aware of and control their anal sphincter muscles. Surgery may be necessary in some cases, such as to repair damaged or weakened anal sphincter muscles.
Pelvic Floor Physical Therapy
Pelvic floor physical therapy is a non-invasive treatment option that involves exercises and techniques to strengthen the anal sphincter muscles and improve their function. This type of therapy can help to improve fecal continence and reduce symptoms of fecal incontinence. Pelvic floor physical therapy may involve exercises such as Kegel exercises, which involve contracting and releasing the anal sphincter muscles to strengthen them.
In addition to exercises, pelvic floor physical therapy may also involve the use of specialized equipment, such as biofeedback devices, to help patients become aware of and control their anal sphincter muscles. Biofeedback devices use sensors to detect the electrical activity of the anal sphincter muscles, and provide feedback to the patient in the form of visual or auditory signals. This feedback can help patients to learn how to control their anal sphincter muscles and improve their function.
What are the symptoms of anal sphincter muscle dysfunction?
+Symptoms of anal sphincter muscle dysfunction may include involuntary loss of stool, pain and bleeding during defecation, and chronic infection and drainage.
How is anal sphincter muscle dysfunction diagnosed?
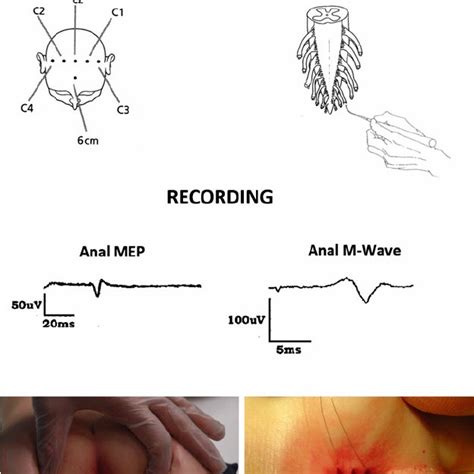
+Diagnosis of anal sphincter muscle dysfunction typically involves a physical examination, medical history, and diagnostic tests such as anal manometry and ultrasound.
What are the treatment options for anal sphincter muscle dysfunction?
+Treatment options for anal sphincter muscle dysfunction depend on the underlying cause and severity of the condition, and may include pelvic floor physical therapy, biofeedback, and surgery.
In conclusion, the anal sphincter muscles play a critical role in maintaining fecal continence and enabling the controlled passage of stool from the body. Dysfunction of these muscles can have significant impacts on quality of life, and treatment options such as pelvic floor physical therapy, biofeedback, and surgery can help to restore normal function to the anal sphincter muscles and alleviate symptoms of fecal incontinence and other conditions. By understanding the anatomy and function of the anal sphincter muscles, as well as the treatment options available, patients can take the first step towards regaining control over their bowel function and improving their overall health and well-being.