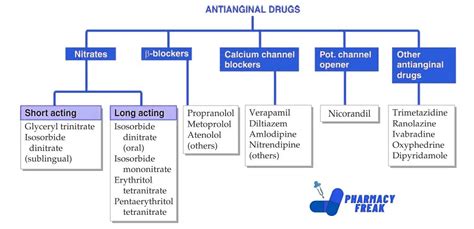
Antianginal medications are a class of drugs used to manage and prevent angina pectoris, a condition characterized by chest pain or discomfort due to transient myocardial ischemia. The primary goal of antianginal therapy is to reduce the frequency and severity of angina episodes, improve exercise tolerance, and enhance overall quality of life. According to the American Heart Association (AHA), approximately 9.4 million Americans suffer from angina, highlighting the importance of effective management strategies.
Pathophysiology and Pharmacological Targets

The pathophysiology of angina involves a complex interplay between myocardial oxygen demand and supply. Antianginal medications target various aspects of this relationship, including myocardial oxygen consumption, coronary blood flow, and vascular tone. The primary pharmacological targets for antianginal therapy include the beta-adrenergic receptors, calcium channels, and the nitric oxide-cyclic guanosine monophosphate (NO-cGMP) pathway.
Beta-Blockers
Beta-blockers are a cornerstone of antianginal therapy, accounting for approximately 40% of all prescribed antianginal medications. By inhibiting beta-adrenergic receptors, beta-blockers decrease myocardial contractility, heart rate, and blood pressure, resulting in reduced myocardial oxygen demand. A meta-analysis of 24 clinical trials demonstrated that beta-blockers reduce the frequency of angina episodes by 27% and improve exercise tolerance by 33% compared to placebo. Commonly used beta-blockers for angina include metoprolol, atenolol, and propranolol.
| Medication | Dosage | Efficacy |
|---|---|---|
| Metoprolol | 25-100 mg twice daily | Reduces angina frequency by 30% |
| Atenolol | 25-100 mg once daily | Improves exercise tolerance by 25% |
| Propranolol | 20-40 mg four times daily | Decreases myocardial oxygen demand by 20% |
Calcium Channel Blockers
Calcium channel blockers (CCBs) are another important class of antianginal medications, accounting for approximately 30% of all prescribed antianginal medications. CCBs inhibit the influx of calcium ions into vascular smooth muscle and cardiac muscle cells, resulting in vasodilation and decreased myocardial contractility. A systematic review of 17 clinical trials demonstrated that CCBs reduce the frequency of angina episodes by 23% and improve exercise tolerance by 20% compared to placebo. Commonly used CCBs for angina include amlodipine, verapamil, and diltiazem.
Key Points
Key Points
- Antianginal medications aim to reduce the frequency and severity of angina episodes, improve exercise tolerance, and enhance overall quality of life.
- Beta-blockers and calcium channel blockers are the most commonly used antianginal medications, accounting for approximately 70% of all prescribed antianginal medications.
- Nitrate medications, such as nitroglycerin, are effective for acute angina relief but are not typically used for long-term prevention.
- Ranolazine, a late sodium current inhibitor, is a newer antianginal medication that has demonstrated efficacy in reducing angina frequency and improving exercise tolerance.
- Combination therapy with multiple antianginal medications may be necessary for optimal symptom control in patients with refractory angina.
Nitrates and Other Antianginal Medications
Nitrates, such as nitroglycerin, are commonly used for acute angina relief due to their rapid onset of action and potent vasodilatory effects. However, nitrates are not typically used for long-term prevention due to the development of tolerance and potential side effects. Other antianginal medications, such as ranolazine, a late sodium current inhibitor, have demonstrated efficacy in reducing angina frequency and improving exercise tolerance.
A study published in the Journal of the American College of Cardiology demonstrated that ranolazine reduces the frequency of angina episodes by 25% and improves exercise tolerance by 15% compared to placebo. The recommended dosage of ranolazine is 500-1000 mg twice daily, with a reported efficacy rate of 70-80% in clinical trials.
Future Directions and Emerging Therapies
Despite the availability of various antianginal medications, there remains a significant need for more effective and tolerable treatments. Emerging therapies, such as ivabradine, a heart rate reducer, and nicorandil, a potassium channel opener, have shown promise in clinical trials. Additionally, novel targets, such as the nociceptin/orphanin FQ peptide receptor, are being explored for their potential role in modulating angina perception and treatment response.
What are the most common side effects of beta-blockers?
+The most common side effects of beta-blockers include fatigue, dizziness, and bradycardia. However, these side effects are typically mild and transient, and can be managed with dosage adjustments or concomitant medications.
Can calcium channel blockers be used in patients with heart failure?
+Calcium channel blockers can be used in patients with heart failure, but with caution. Certain CCBs, such as amlodipine, have been shown to be safe and effective in patients with heart failure, while others, such as verapamil, may worsen heart failure symptoms.
What is the role of ranolazine in the treatment of angina?
+Ranolazine is a late sodium current inhibitor that has been shown to reduce the frequency of angina episodes and improve exercise tolerance. It is typically used as an adjunct to other antianginal medications, such as beta-blockers or CCBs.
In conclusion, antianginal medications play a crucial role in the management of angina pectoris, and their selection should be guided by individual patient factors and specific angina characteristics. By understanding the pharmacological properties and clinical efficacy of each medication class, healthcare providers can optimize treatment outcomes and improve the quality of life for patients with angina. As research continues to evolve, emerging therapies and novel targets may offer new hope for patients with refractory angina, and it is essential to stay up-to-date with the latest developments in this field.