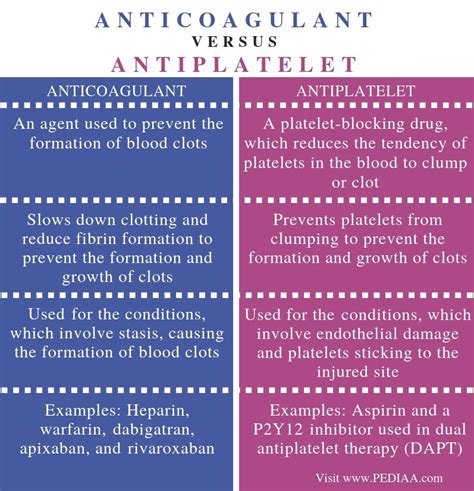
The realm of cardiovascular medicine has witnessed significant advancements in the prevention and treatment of thrombotic disorders, with anticoagulants and antiplatelets being two cornerstone therapies. While both classes of drugs aim to prevent the formation of blood clots, they operate through distinct mechanisms, possess different indications, and carry unique risks and benefits. Understanding the nuances of anticoagulant vs antiplatelet therapy is crucial for clinicians to make informed decisions and for patients to comprehend their treatment regimens.
Introduction to Anticoagulants and Antiplatelets
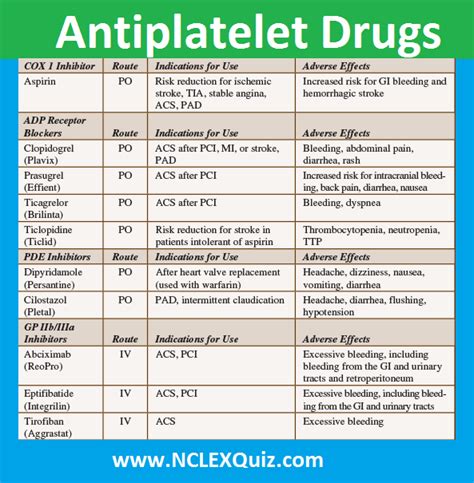
Anticoagulants, also known as blood thinners, are medications that prevent the formation of blood clots by inhibiting the coagulation cascade. This process involves a complex series of enzymatic reactions that ultimately lead to the conversion of fibrinogen into fibrin, forming a blood clot. Anticoagulants can be further divided into traditional agents, such as warfarin, and novel oral anticoagulants (NOACs), including rivaroxaban, apixaban, and dabigatran. On the other hand, antiplatelets are drugs that inhibit platelet activation and aggregation, which are critical steps in the formation of arterial thrombi. Aspirin is the most well-known antiplatelet agent, but other examples include clopidogrel, prasugrel, and ticagrelor.
Key Points
- Anticoagulants prevent blood clot formation by inhibiting the coagulation cascade.
- Antiplatelets inhibit platelet activation and aggregation, primarily used in arterial thrombosis prevention.
- Warfarin and NOACs are types of anticoagulants, while aspirin and P2Y12 inhibitors are types of antiplatelets.
- The choice between anticoagulant and antiplatelet therapy depends on the specific clinical indication, patient risk factors, and potential for bleeding complications.
- Combination therapy with both anticoagulants and antiplatelets may be used in certain clinical scenarios, such as atrial fibrillation with coronary artery disease.
Mechanisms of Action
The mechanisms of action of anticoagulants and antiplatelets underpin their therapeutic effects and side effect profiles. Anticoagulants can target various steps in the coagulation cascade. For instance, warfarin inhibits the synthesis of vitamin K-dependent clotting factors (II, VII, IX, and X), while NOACs directly inhibit either factor Xa (e.g., rivaroxaban) or thrombin (e.g., dabigatran). In contrast, antiplatelets primarily target the platelet activation and aggregation pathway. Aspirin irreversibly inhibits cyclooxygenase-1 (COX-1), reducing thromboxane A2 production, a potent platelet activator. P2Y12 inhibitors, such as clopidogrel, block the P2Y12 receptor on platelets, preventing adenosine diphosphate (ADP)-mediated platelet activation and aggregation.
| Drug Class | Mechanism of Action | Examples |
|---|---|---|
| Anticoagulants | Inhibit coagulation cascade | Warfarin, Rivaroxaban, Apixaban, Dabigatran |
| Antiplatelets | Inhibit platelet activation and aggregation | Aspirin, Clopidogrel, Prasugrel, Ticagrelor |
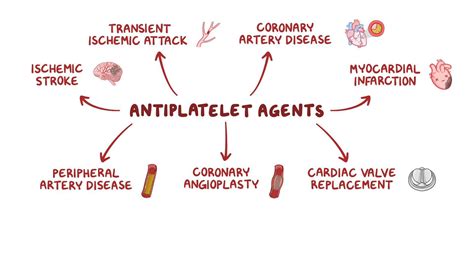
Clinical Indications and Usage
The clinical indications for anticoagulants and antiplatelets differ, reflecting their distinct mechanisms of action and the nature of the thrombotic disorders they are designed to prevent or treat. Anticoagulants are primarily used in the prevention and treatment of venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), as well as in the prevention of stroke in patients with atrial fibrillation not caused by heart valve problems. Antiplatelets, on the other hand, are mainly used in the prevention of arterial thrombotic events, such as myocardial infarction (MI) and ischemic stroke, particularly in patients with a history of coronary artery disease or those undergoing coronary stenting.
Risk of Bleeding and Monitoring
Both anticoagulants and antiplatelets increase the risk of bleeding, which can range from minor bruising to life-threatening hemorrhage. The risk of bleeding with anticoagulants is generally higher than with antiplatelets, particularly with warfarin, which requires regular monitoring of the international normalized ratio (INR) to ensure therapeutic anticoagulation without excessive risk of bleeding. NOACs have a more predictable pharmacokinetic profile and do not require routine monitoring, although their use is not without bleeding risk. Antiplatelets also carry a bleeding risk, but it is generally lower than that associated with anticoagulants. However, the combination of anticoagulants and antiplatelets in certain clinical scenarios can significantly increase the risk of bleeding, necessitating careful consideration and monitoring.
What is the primary difference between anticoagulants and antiplatelets?
+Anticoagulants prevent blood clot formation by inhibiting the coagulation cascade, while antiplatelets inhibit platelet activation and aggregation, primarily used in arterial thrombosis prevention.
Which conditions are anticoagulants typically used for?
+Anticoagulants are used in the prevention and treatment of venous thromboembolism (VTE) and the prevention of stroke in patients with atrial fibrillation not caused by heart valve problems.
What is the role of monitoring in patients on anticoagulant therapy?
+Monitoring, such as INR for warfarin, is crucial to ensure therapeutic anticoagulation levels are maintained without excessively increasing the risk of bleeding.
In conclusion, the distinction between anticoagulants and antiplatelets is fundamental to the practice of cardiovascular medicine. By understanding their mechanisms of action, clinical indications, and risks, clinicians can provide personalized care that balances the prevention of thrombotic events against the risk of bleeding. As the field continues to evolve with the development of new agents and therapeutic strategies, the core principles of anticoagulant and antiplatelet therapy will remain essential for improving patient outcomes.