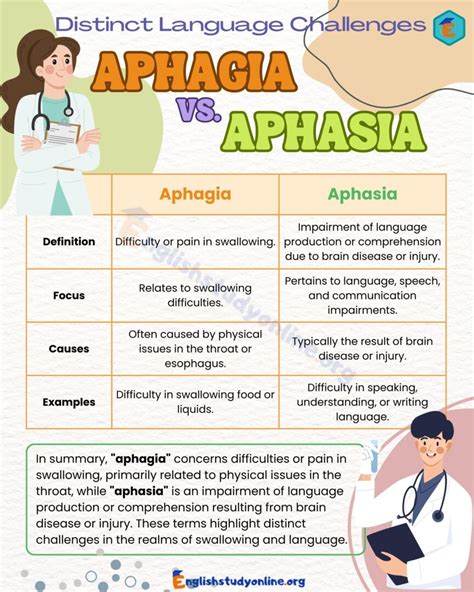
Aphagia, a condition characterized by the inability to swallow, is a complex disorder that affects individuals in various ways. While it shares some similarities with other swallowing disorders, such as dysphagia, aphagia has distinct differences that set it apart. In this article, we will explore 5 ways aphagia differs from other conditions, highlighting its unique characteristics and implications for diagnosis and treatment.
Key Points
- Aphagia is a distinct condition from dysphagia, with a focus on the inability to initiate swallowing rather than difficulty swallowing.
- Aphagia often results from neurological or muscular disorders, such as stroke, cerebral palsy, or amyotrophic lateral sclerosis (ALS).
- The condition can lead to severe complications, including malnutrition, dehydration, and aspiration pneumonia.
- Treatment for aphagia typically involves a multidisciplinary approach, incorporating strategies from speech-language pathology, occupational therapy, and nutrition.
- Early diagnosis and intervention are critical in managing aphagia, as prompt treatment can significantly improve quality of life and reduce the risk of complications.
1. Etiology and Pathophysiology
Aphagia differs from other swallowing disorders in its underlying causes and pathophysiological mechanisms. While dysphagia can result from a range of factors, including anatomical abnormalities, neurological disorders, or gastrointestinal conditions, aphagia is often associated with specific neurological or muscular disorders. For example, stroke, cerebral palsy, and amyotrophic lateral sclerosis (ALS) are common underlying conditions that can lead to aphagia. Understanding the distinct etiology and pathophysiology of aphagia is essential for developing effective treatment strategies.
Neurological Basis of Aphagia
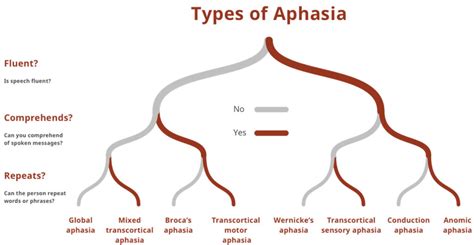
The neurological basis of aphagia involves the disruption of complex neural networks responsible for controlling swallowing. Research has shown that the brainstem and cerebral cortex play critical roles in regulating swallowing, and damage to these areas can result in aphagia. Furthermore, electrophysiological studies have demonstrated that individuals with aphagia often exhibit abnormal patterns of neural activity, including delayed or absent swallowing responses.
| Condition | Underlying Cause | Pathophysiological Mechanism |
|---|---|---|
| Aphagia | Neurological or muscular disorders | Disruption of neural networks controlling swallowing |
| Dysphagia | Anatomical abnormalities, neurological disorders, or gastrointestinal conditions | Obstruction or dysfunction of the swallowing mechanism |
2. Clinical Presentation and Diagnosis
Aphagia presents with distinct clinical features that differentiate it from other swallowing disorders. Individuals with aphagia often exhibit inability to initiate swallowing, food refusal, and aspiration. Diagnosis of aphagia typically involves a comprehensive evaluation, including medical history, physical examination, swallowing assessment, and imaging studies. A thorough understanding of the clinical presentation and diagnostic criteria is essential for accurate diagnosis and effective management of aphagia.
Diagnostic Challenges
Diagnosing aphagia can be challenging, as the condition often presents with non-specific symptoms. Differential diagnosis is essential to rule out other conditions that may mimic aphagia, such as gastroesophageal reflux disease (GERD) or esophageal dysmotility. Clinicians should employ a combination of diagnostic tools, including videofluoroscopic swallowing studies (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES), to confirm the diagnosis and develop an effective treatment plan.
3. Complications and Consequences
Aphagia can lead to severe complications, including malnutrition, dehydration, and aspiration pneumonia. The condition can also result in respiratory complications, such as chronic obstructive pulmonary disease (COPD) or pneumonia. Understanding the potential complications and consequences of aphagia is essential for developing effective treatment strategies and improving patient outcomes.
Impact on Quality of Life
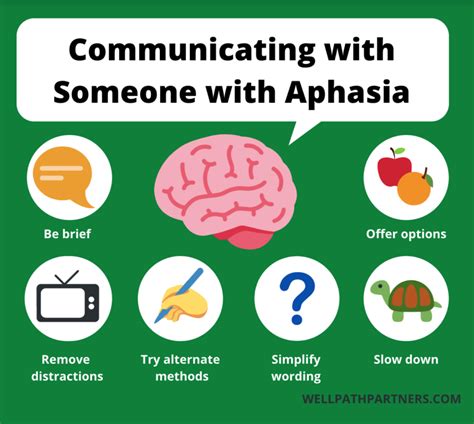
Aphagia can significantly impact an individual’s quality of life, leading to social isolation, anxiety, and depression. The condition can also result in cognitive impairment and functional decline, further compromising the individual’s overall well-being. Clinicians should prioritize patient-centered care and employ a multidisciplinary approach to address the complex needs of individuals with aphagia.
4. Treatment and Management
Treatment for aphagia typically involves a multidisciplinary approach, incorporating strategies from speech-language pathology, occupational therapy, and nutrition. Clinicians should employ a combination of behavioral interventions, such as swallowing exercises and feeding techniques, and medical management, including medications and nutritional supplements. Understanding the distinct treatment needs of individuals with aphagia is essential for developing effective management strategies.
Role of Technology in Aphagia Management
Technology can play a critical role in the management of aphagia, particularly in the development of assistive devices and communication aids. For example, electronic swallowing devices can help individuals with aphagia initiate swallowing, while augmentative and alternative communication (AAC) devices can facilitate communication and reduce social isolation.
5. Prognosis and Future Directions
The prognosis for individuals with aphagia is variable, depending on the underlying cause and severity of the condition. Early diagnosis and intervention are critical in improving outcomes and reducing the risk of complications. Future research should focus on developing novel treatments and interventions for aphagia, including stem cell therapy and gene therapy. Clinicians should prioritize patient-centered care and employ a multidisciplinary approach to address the complex needs of individuals with aphagia.
What is the primary difference between aphagia and dysphagia?
+Aphagia is characterized by the inability to initiate swallowing, while dysphagia refers to difficulty swallowing. Understanding this distinction is essential for accurate diagnosis and effective management of these conditions.
What are the common underlying causes of aphagia?
+Aphagia often results from neurological or muscular disorders, such as stroke, cerebral palsy, or amyotrophic lateral sclerosis (ALS). Understanding the underlying cause of aphagia is critical for developing effective treatment strategies.
How can aphagia be diagnosed?
+Diagnosis of aphagia typically involves a comprehensive evaluation, including medical history, physical examination, swallowing assessment, and imaging studies. A thorough understanding of the clinical presentation and diagnostic criteria is essential for accurate diagnosis and effective management of aphagia.