Antibiotics are a crucial part of modern medicine, helping to combat bacterial infections and save countless lives. However, like all medications, they can have side effects, some of which can be quite uncomfortable. One of the lesser-known but still significant side effects of antibiotics is constipation. In this article, we’ll delve into the relationship between antibiotics and constipation, exploring why this happens, which antibiotics are more likely to cause constipation, and what you can do to manage or prevent this side effect.
Understanding Antibiotics and Their Effects on the Body
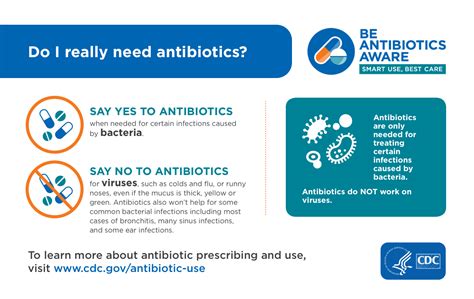
Antibiotics work by targeting and killing bacteria that cause infections. However, they can also affect the balance of bacteria in your gut, which is essential for proper digestion and bowel movements. The human gut is home to trillions of microorganisms, known as the gut microbiome, which plays a critical role in digestion, immune system function, and even mental health. When antibiotics disrupt this balance, it can lead to various gastrointestinal symptoms, including constipation.
Constipation, characterized by infrequent bowel movements, hard or lumpy stools, and difficulty passing stools, can be quite distressing. It's essential to understand that while antibiotics can cause constipation, not everyone who takes antibiotics will experience this side effect. The likelihood and severity of constipation can depend on several factors, including the type of antibiotic, the duration of treatment, and individual differences in gut microbiota.
Which Antibiotics Are More Likely to Cause Constipation?
Not all antibiotics are equal when it comes to their potential to cause constipation. Some classes of antibiotics are more likely to disrupt the gut microbiome and lead to constipation than others. For example, broad-spectrum antibiotics, which target a wide range of bacteria, are more likely to cause constipation because they can kill off both harmful and beneficial bacteria in the gut. Specific examples include:
- Macrolides (such as erythromycin and azithromycin)
- Fluoroquinolones (such as ciprofloxacin and levofloxacin)
- Cephalosporins (such as cefalexin and ceftriaxone)
| Antibiotic Class | Examples | Potential for Constipation |
|---|---|---|
| Macrolides | Erythromycin, Azithromycin | High |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | High |
| Cephalosporins | Cefalexin, Ceftriaxone | Moderate to High |
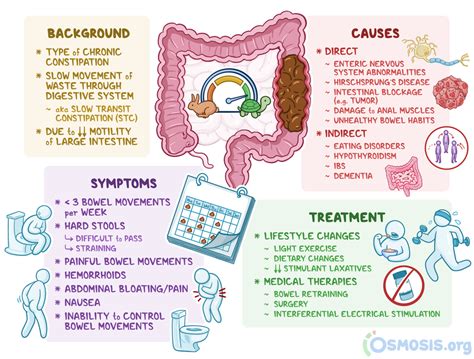
Managing Constipation Caused by Antibiotics

If you’re taking antibiotics and experience constipation, there are several steps you can take to manage this side effect. Here are some strategies:
- Stay Hydrated: Drinking plenty of water can help soften stool and make it easier to pass.
- Increase Fiber Intake: Foods high in fiber, such as fruits, vegetables, and whole grains, can help promote regular bowel movements.
- Exercise Regularly: Physical activity can help stimulate bowel movements.
- Consider Probiotics: Probiotics are beneficial bacteria that can help restore the balance of the gut microbiome. They are available in fermented foods like yogurt and kefir, as well as in supplement form. However, it’s essential to consult with your healthcare provider before starting any supplements.
It's also important to note that if your constipation is severe or accompanied by other symptoms such as abdominal pain, blood in the stool, or fever, you should seek medical attention. Your healthcare provider may need to adjust your antibiotic regimen or prescribe additional medications to manage your symptoms.
Key Points
- Antibiotics can disrupt the balance of the gut microbiome, leading to constipation.
- Not all antibiotics have the same risk of causing constipation; broad-spectrum antibiotics are more likely to cause this side effect.
- Staying hydrated, increasing fiber intake, exercising regularly, and considering probiotics can help manage constipation caused by antibiotics.
- If constipation is severe or accompanied by other concerning symptoms, seek medical attention.
- Individual responses to antibiotics can vary, and the likelihood of experiencing constipation depends on several factors, including the type of antibiotic and individual differences in gut health.
Looking Ahead: Preventing Constipation with Antibiotics
While antibiotics are sometimes necessary to treat bacterial infections, preventing constipation whenever possible can make the treatment process more comfortable. Besides the strategies mentioned for managing constipation, maintaining a healthy diet rich in fiber, staying well-hydrated, and engaging in regular physical activity before starting antibiotics can help minimize the risk of developing constipation.
Furthermore, researchers are continually exploring new antibiotics and treatment strategies that have fewer side effects, including those that target specific bacteria without broadly affecting the gut microbiome. The development of such targeted therapies could reduce the incidence of antibiotic-associated constipation in the future.
Can all antibiotics cause constipation?
+No, not all antibiotics are equally likely to cause constipation. Broad-spectrum antibiotics are more likely to disrupt the gut microbiome and lead to constipation.
How can I prevent constipation while taking antibiotics?
+Staying hydrated, eating a diet high in fiber, exercising regularly, and considering probiotics can help prevent or manage constipation caused by antibiotics.
Should I stop taking my antibiotics if I experience constipation?
+No, you should not stop taking your antibiotics without consulting your healthcare provider. They can assess your situation and provide guidance on managing constipation while ensuring your infection is properly treated.
In conclusion, while antibiotics can cause constipation as a side effect, understanding which antibiotics are more likely to cause this issue and taking proactive steps to manage gut health can make a significant difference. By being informed and working closely with your healthcare provider, you can navigate the potential side effects of antibiotics and ensure that your treatment is as effective and comfortable as possible.



