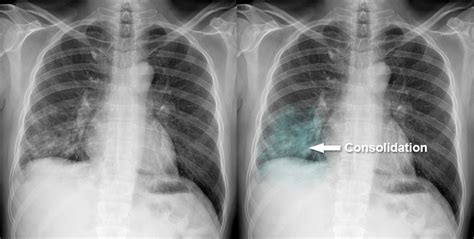
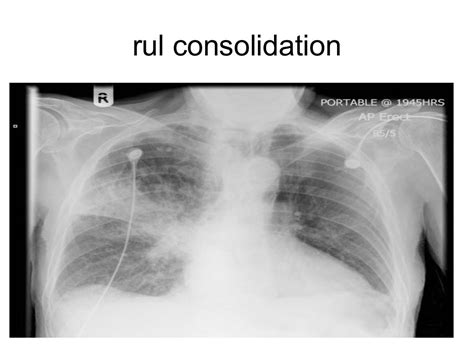
The consolidation of lung refers to a condition where the lung tissue becomes solid and firm due to the accumulation of fluid, cells, or other substances, replacing the normal air-filled spaces. This can be caused by a variety of factors, including infections, inflammation, and injury. In medical imaging, consolidation is often seen on chest X-rays or computed tomography (CT) scans, where it appears as a homogeneous area of increased density. Understanding the causes, symptoms, and diagnosis of lung consolidation is crucial for effective management and treatment.
One of the primary causes of lung consolidation is pneumonia, which is an infection of the lungs caused by bacteria, viruses, or fungi. When an infectious agent enters the lungs, it can trigger an inflammatory response, leading to the accumulation of fluid, white blood cells, and other debris in the air-filled spaces of the lungs. This results in the consolidation of lung tissue, which can impair gas exchange and lead to respiratory symptoms such as cough, fever, and shortness of breath. Other causes of lung consolidation include pulmonary edema, where fluid accumulates in the lungs due to heart failure or high altitude, and hemorrhage, where bleeding into the lungs can cause consolidation.
Key Points
- Lung consolidation is a condition where lung tissue becomes solid and firm due to the accumulation of fluid, cells, or other substances.
- Pneumonia is a primary cause of lung consolidation, resulting from an infection of the lungs by bacteria, viruses, or fungi.
- Symptoms of lung consolidation include cough, fever, shortness of breath, and chest pain.
- Diagnosis of lung consolidation involves medical imaging, such as chest X-rays or CT scans, and laboratory tests, including blood cultures and sputum analysis.
- Treatment of lung consolidation depends on the underlying cause and may include antibiotics, antiviral medications, oxygen therapy, and supportive care.
Causes and Risk Factors
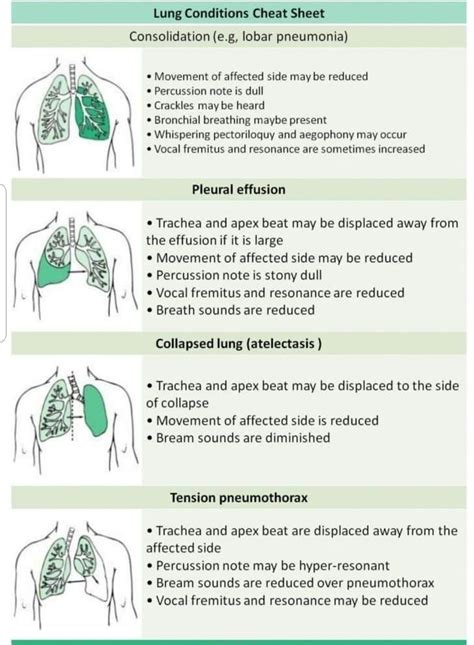
The causes of lung consolidation can be diverse, ranging from infectious agents to non-infectious conditions. In addition to pneumonia, other infections such as bronchiectasis, where the airways are permanently enlarged, and lung abscesses, where a pocket of pus forms in the lungs, can cause consolidation. Non-infectious causes include pulmonary embolism, where a blood clot blocks an artery in the lungs, and acute respiratory distress syndrome (ARDS), where inflammation and injury to the lungs can lead to consolidation.
Pathophysiology
The pathophysiology of lung consolidation involves the disruption of the normal air-filled spaces in the lungs, leading to impaired gas exchange and respiratory symptoms. When the lungs become consolidated, the alveoli, which are the tiny air sacs where gas exchange occurs, become filled with fluid or other substances, reducing the surface area available for oxygen and carbon dioxide exchange. This can lead to hypoxemia, where the level of oxygen in the blood is low, and hypercapnia, where the level of carbon dioxide in the blood is high.
| Condition | Description | Clinical Features |
|---|---|---|
| Pneumonia | Infection of the lungs by bacteria, viruses, or fungi | Cough, fever, shortness of breath, chest pain |
| Pulmonary Edema | Fluid accumulation in the lungs due to heart failure or high altitude | Shortness of breath, cough, orthopnea, paroxysmal nocturnal dyspnea |
| Acute Respiratory Distress Syndrome (ARDS) | Inflammation and injury to the lungs, leading to consolidation | Shortness of breath, hypoxemia, hypercapnia, respiratory failure |
Diagnosis and Treatment
The diagnosis of lung consolidation involves a combination of clinical evaluation, medical imaging, and laboratory tests. A physical examination and medical history can provide clues to the underlying cause, while chest X-rays and CT scans can help identify areas of consolidation. Laboratory tests, such as blood cultures and sputum analysis, can help identify the causative agent and guide treatment.
Treatment Options
The treatment of lung consolidation depends on the underlying cause. For infectious causes, antibiotics or antiviral medications may be prescribed, while for non-infectious causes, treatment may involve supportive care, such as oxygen therapy and respiratory support. In severe cases, mechanical ventilation may be required to support respiratory function.
In conclusion, lung consolidation is a serious condition that requires prompt diagnosis and treatment. Understanding the causes, symptoms, and diagnosis of lung consolidation is crucial for effective management and treatment. By recognizing the signs and symptoms of lung consolidation and seeking medical attention early, individuals can reduce the risk of complications and improve outcomes.
What are the symptoms of lung consolidation?
+The symptoms of lung consolidation include cough, fever, shortness of breath, and chest pain.
How is lung consolidation diagnosed?
+Lung consolidation is diagnosed through a combination of clinical evaluation, medical imaging, and laboratory tests, including chest X-rays, CT scans, blood cultures, and sputum analysis.
What is the treatment for lung consolidation?
+The treatment for lung consolidation depends on the underlying cause and may include antibiotics, antiviral medications, oxygen therapy, and supportive care.