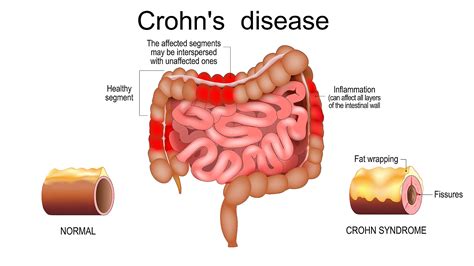
Crohn's disease, a type of inflammatory bowel disease (IBD), affects millions of people worldwide, causing symptoms such as abdominal pain, diarrhea, fatigue, weight loss, and malnutrition. The management of Crohn's disease often involves a combination of medication, lifestyle changes, and in some cases, surgery. Medications play a crucial role in controlling the symptoms, inducing and maintaining remission, and improving the quality of life for patients with Crohn's disease. Understanding the different types of Crohn's medications, their mechanisms of action, potential side effects, and the factors that influence their prescription is essential for both patients and healthcare providers.
Key Points
- Crohn's disease is a chronic inflammatory bowel disease that requires long-term management.
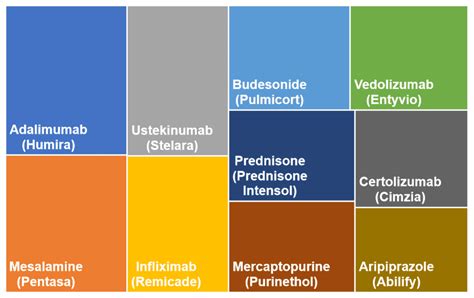
- Medications for Crohn's disease are classified into several categories, including aminosalicylates, corticosteroids, immunomodulators, biologics, and JAK inhibitors.
- The choice of medication depends on the severity of the disease, the extent of the disease, and the patient's response to previous treatments.
- Lifestyle changes, such as dietary modifications and stress management, can complement medication therapy.
- Regular monitoring and follow-up with a healthcare provider are crucial to adjust the treatment plan as needed and manage potential side effects.
Classification of Crohn’s Medications
Crohn’s medications can be broadly classified into several categories based on their mechanism of action and therapeutic effects. These categories include aminosalicylates, corticosteroids, immunomodulators, biologics, and JAK inhibitors. Each category has its specific indications, dosages, and side effect profiles.
Aminosalicylates
Aminosalicylates, such as sulfasalazine and mesalamine, are often used as the first line of treatment for mild to moderate Crohn’s disease. They work by reducing inflammation in the gastrointestinal tract. These medications are particularly effective for patients with colonic involvement and can be administered orally or rectally, depending on the extent and location of the disease.
Corticosteroids
Corticosteroids, including prednisone and budesonide, are potent anti-inflammatory agents used to induce remission in patients with moderate to severe Crohn’s disease. They can be given orally or intravenously, depending on the severity of the symptoms. However, due to their significant side effects, corticosteroids are generally used for short-term therapy to control acute flare-ups.
Immunomodulators
Immunomodulators, such as azathioprine and mercaptopurine, are used to maintain remission in patients with Crohn’s disease, especially those who are steroid-dependent or have failed to respond to aminosalicylates. These medications work by suppressing the immune system, thereby reducing inflammation. They are typically used in combination with other medications and require regular monitoring due to potential side effects.
Biologics
Biologic therapies, including tumor necrosis factor-alpha (TNF-alpha) inhibitors (e.g., infliximab, adalimumab, and certolizumab), interleukin-12 and -23 inhibitors (e.g., ustekinumab), and integrin receptor blockers (e.g., vedolizumab), have revolutionized the treatment of Crohn’s disease. Biologics target specific molecules involved in the inflammatory process, offering a more targeted approach to treatment. They are particularly useful for patients who have not responded to conventional therapies or have fistulizing disease.
JAK Inhibitors
Janus kinase (JAK) inhibitors, such as tofacitinib, represent a newer class of medications for the treatment of Crohn’s disease. They work by inhibiting the JAK pathway, which is involved in the body’s immune response. JAK inhibitors offer an oral treatment option for patients with moderate to severe Crohn’s disease who have failed or are intolerant to other therapies.
| Medication Category | Examples | Indications |
|---|---|---|
| Aminosalicylates | Sulfasalazine, Mesalamine | Mild to moderate Crohn's disease |
| Corticosteroids | Prednisone, Budesonide | Moderate to severe Crohn's disease, acute flare-ups |
| Immunomodulators | Azathioprine, Mercaptopurine | Maintenance of remission, steroid-dependent patients |
| Biologics | Infliximab, Adalimumab, Ustekinumab | Patients not responding to conventional therapies, fistulizing disease |
| JAK Inhibitors | Tofacitinib | Moderate to severe Crohn's disease, patients who have failed other therapies |
Lifestyle Modifications and Supportive Care

Beyond medication, lifestyle modifications play a significant role in managing Crohn’s disease. A balanced diet, adequate hydration, stress management techniques, and regular physical activity can help alleviate symptoms and improve quality of life. Additionally, supportive care, including psychological support and patient education, is essential for coping with the chronic nature of the disease.
Nutritional Management
Nutritional therapy is a critical component of Crohn’s disease management. Patients may require specific diets tailored to their needs, such as a low-residue diet during flare-ups or nutritional supplements to address malabsorption and deficiencies. Enteral nutrition, where nutrients are delivered directly into the gastrointestinal tract, can be beneficial, especially in pediatric patients or those with severe malnutrition.
Psychological Support
Crohn’s disease can have a profound impact on a patient’s mental health and well-being. Psychological support, including counseling and support groups, can help patients cope with the emotional aspects of living with a chronic illness. Mindfulness techniques, such as meditation and yoga, can also be beneficial in managing stress and improving overall well-being.
What are the common side effects of Crohn's medications?
+Common side effects of Crohn's medications can include nausea, vomiting, diarrhea, abdominal pain, and increased risk of infections. More severe side effects, such as allergic reactions, liver damage, and increased risk of certain cancers, can also occur. Regular monitoring by a healthcare provider is essential to manage these side effects.
How long does it take for Crohn's medications to start working?
+The time it takes for Crohn's medications to start working can vary depending on the type of medication and the individual patient. Some medications, like corticosteroids, can start to work within a few days, while others, such as biologics, may take several weeks to a few months to show their full effects.
Can Crohn's disease be cured with medication?
+Currently, there is no cure for Crohn's disease. However, with the right combination of medications and lifestyle modifications, many patients can achieve and maintain remission, significantly improving their quality of life.
In conclusion, the management of Crohn’s disease involves a multifaceted approach, incorporating medication, lifestyle modifications, and supportive care. By understanding the various types of medications available, their potential side effects, and the importance of personalized treatment plans, patients and healthcare providers can work together to achieve the best possible outcomes and improve the quality of life for those living with Crohn’s disease.