Medicaid, a joint federal and state program, provides health coverage to millions of Americans, including low-income individuals, families, and children, as well as pregnant women, elderly adults, and people with disabilities. One of the essential aspects of healthcare that Medicaid covers is hearing health, which includes the cost of hearing aids for eligible beneficiaries. However, the extent of coverage for hearing aids under Medicaid varies significantly from state to state, reflecting the program's structure, which allows states considerable flexibility in designing their Medicaid benefits packages.
Understanding Medicaid Coverage for Hearing Aids

The coverage of hearing aids by Medicaid is influenced by federal regulations and state-specific policies. At the federal level, Medicaid requires states to provide certain mandatory benefits, including doctor visits, hospital stays, and vaccinations. However, the coverage of hearing aids, including the devices themselves and the related services such as fittings and follow-up care, falls under optional benefits. This means that while states are not required to cover hearing aids, many do so as part of their optional benefits, recognizing the importance of hearing health for overall well-being and quality of life.
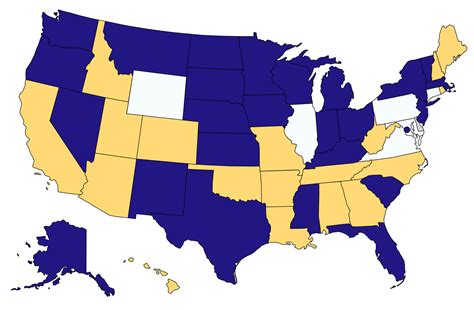
State Variations in Coverage
A critical aspect of Medicaid coverage for hearing aids is the variability among states. Some states provide comprehensive coverage for hearing aids, including the cost of the devices, evaluations, fittings, and repairs, for all eligible beneficiaries. In contrast, other states may limit coverage to specific populations, such as children, or may impose restrictions on the types of hearing aids covered or the frequency of replacement. For example, some states may cover hearing aids only for children under a certain age or may require a specific medical necessity criteria to be met before approving coverage for adults.
| State | Coverage Details |
|---|---|
| California | Covers hearing aids for children and adults with a medical necessity determination. |
| New York | Provides coverage for hearing aids for all eligible beneficiaries, including adults and children, with certain limitations on device type and frequency of replacement. |
| Texas | Limits coverage to children under 21 years of age, with specific requirements for medical necessity and prior authorization. |

Eligibility and Application Process
To be eligible for Medicaid coverage of hearing aids, individuals must first qualify for Medicaid. Eligibility is based on income and family size, among other factors, and varies by state. Once eligible for Medicaid, beneficiaries can apply for hearing aid coverage by contacting their state’s Medicaid agency or a participating healthcare provider. The application process typically involves a hearing evaluation by an audiologist or hearing specialist to determine the medical necessity of a hearing aid. If approved, Medicaid will cover the specified benefits according to the state’s coverage policies.
Importance of Early Intervention
Early intervention is crucial for individuals, especially children, with hearing loss. Untreated hearing loss can lead to significant delays in speech and language development, as well as social and emotional difficulties. Medicaid coverage for hearing aids plays a vital role in ensuring that eligible children and adults receive necessary hearing healthcare services, thereby mitigating the potential long-term impacts of untreated hearing loss.
Key Points
- Medicaid coverage for hearing aids varies by state, with some states providing comprehensive coverage and others limiting it to specific populations or imposing restrictions.
- Eligibility for Medicaid and the application process for hearing aid coverage involve income and family size considerations, as well as a medical necessity determination.
- Early intervention is critical for addressing hearing loss, especially in children, to prevent delays in speech and language development and other potential long-term effects.
- Beneficiaries should consult their state's Medicaid program for specific details on hearing aid coverage, including any requirements or limitations that apply.
- The flexibility in Medicaid's structure allows states to design benefits that meet the unique needs of their populations, including the provision of hearing healthcare services.
In conclusion, while Medicaid's coverage of hearing aids is not uniform across all states, the program plays a vital role in ensuring access to hearing healthcare for millions of Americans who might otherwise be unable to afford these essential services. By understanding the specifics of their state's Medicaid program and the eligibility requirements for hearing aid coverage, individuals can navigate the system more effectively and receive the care they need to improve their hearing health and overall quality of life.
How do I find out if my state’s Medicaid program covers hearing aids?
+To find out if your state’s Medicaid program covers hearing aids, you should contact your state’s Medicaid agency directly. They can provide you with the most current and detailed information about hearing aid coverage, including any eligibility requirements, covered services, and limitations.
What is the process for getting a hearing aid covered by Medicaid?
+The process for getting a hearing aid covered by Medicaid typically begins with a hearing evaluation by an audiologist or hearing specialist to determine medical necessity. If the evaluation indicates that a hearing aid is necessary, the provider will submit a request for coverage to the Medicaid program. Beneficiaries may need to provide additional information or meet specific criteria as outlined by their state’s Medicaid program.
Can children with Medicaid receive coverage for hearing aids?
+Yes, many states provide coverage for hearing aids for children under Medicaid. In fact, early intervention services, including hearing aids, are often prioritized for children to address hearing loss and prevent developmental delays. The specifics of coverage, including any age limits or service requirements, vary by state.



