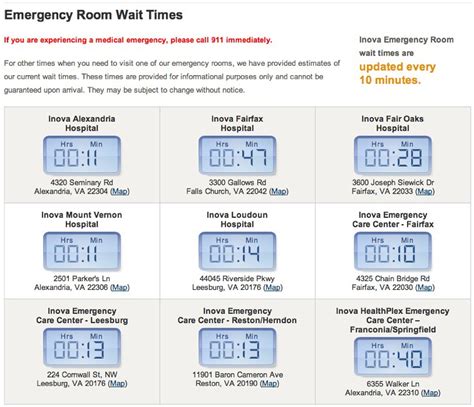
The emergency room (ER) is a critical component of the healthcare system, providing immediate attention to patients with acute injuries or illnesses. However, one of the most significant challenges faced by ERs is managing wait times. Prolonged wait times can lead to decreased patient satisfaction, increased stress for healthcare providers, and potentially life-threatening consequences for patients with severe conditions. According to the Centers for Disease Control and Prevention (CDC), the average wait time in ERs across the United States is approximately 40 minutes, with 1 in 5 patients waiting over an hour to receive care.
Understanding the factors that contribute to ER wait times is essential for developing effective strategies to mitigate them. One primary factor is the volume of patients presenting to the ER, which can fluctuate significantly depending on the time of day, day of the week, and seasonal trends. For instance, ERs tend to experience higher volumes during evenings, weekends, and holidays, as well as during flu season. Additionally, the severity of patient conditions, availability of medical staff, and hospital resource allocation also play significant roles in determining wait times. A study published in the Journal of Emergency Medicine found that ERs with higher patient-to-nurse ratios and those with limited access to diagnostic imaging and laboratory services tend to have longer wait times.
Key Points
- Average ER wait time in the US is approximately 40 minutes, with 1 in 5 patients waiting over an hour.
- Patient volume, severity of conditions, medical staff availability, and hospital resource allocation are key factors influencing ER wait times.
- Effective strategies to reduce wait times include implementing triage systems, optimizing staffing models, and leveraging technology for more efficient patient flow.
- Reducing ER wait times can lead to improved patient satisfaction, better health outcomes, and decreased costs associated with prolonged care.
- Collaboration between healthcare providers, hospital administrators, and policymakers is crucial for addressing the systemic issues contributing to prolonged ER wait times.
Factors Contributing to ER Wait Times
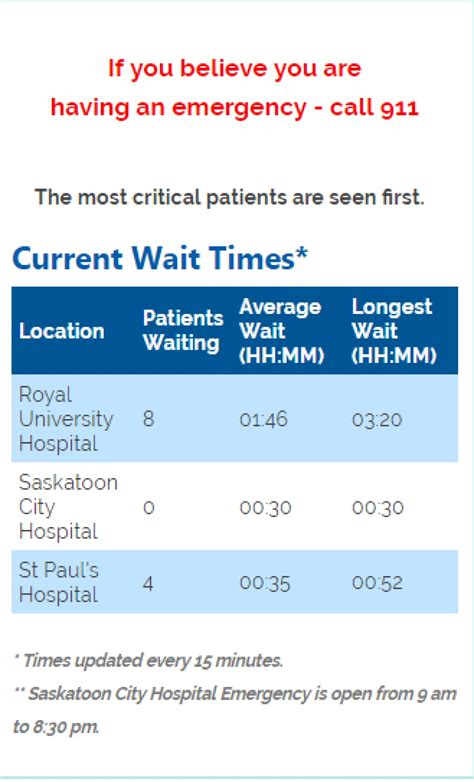
Several factors contribute to ER wait times, including the efficiency of the triage process, the availability of medical staff, and the capacity of the ER to manage patient flow. A well-organized triage system is critical for quickly assessing the severity of patient conditions and prioritizing care accordingly. However, in many ERs, the triage process can be time-consuming and may not always accurately reflect the urgency of patient needs. Moreover, the availability of medical staff, particularly during peak hours, can significantly impact wait times. ERs that are understaffed or have inadequate skill mix among their personnel may struggle to provide timely care.
Triage Systems and Patient Flow
Implementing efficient triage systems and optimizing patient flow are essential for reducing ER wait times. Triage systems that utilize evidence-based criteria, such as the Emergency Severity Index (ESI), can help quickly identify patients who require immediate attention and those who can safely wait. Moreover, strategies that streamline patient flow, such as using “fast track” areas for less severe conditions and implementing bedside registration, can also help decrease wait times. A study published in the Annals of Emergency Medicine found that ERs that implemented a fast track system for patients with minor conditions reduced their overall wait times by an average of 30 minutes.
| ER Wait Time Reduction Strategies | Implementation Challenges |
|---|---|
| Implementing efficient triage systems | Requires significant training for staff and may necessitate additional resources |
| Optimizing staffing models | Can be costly and may require significant changes to existing shift patterns |
| Leveraging technology for patient flow | May require substantial investment in new software and hardware, as well as staff training |
| Enhancing patient communication | Requires a cultural shift towards more patient-centered care and may necessitate additional staff to manage communication |
Consequences of Prolonged ER Wait Times

Prolonged ER wait times can have significant consequences for patients, healthcare providers, and the healthcare system as a whole. For patients, delayed care can lead to worsening of conditions, increased risk of complications, and decreased satisfaction with care. A study published in the Journal of Patient Safety found that patients who experienced longer wait times in the ER were more likely to report dissatisfaction with their care and had higher rates of readmission. For healthcare providers, prolonged wait times can lead to increased stress, burnout, and decreased job satisfaction. Furthermore, from a systemic perspective, prolonged ER wait times can result in increased costs associated with prolonged care, as well as potential legal and reputational risks for hospitals.
Strategies for Reducing ER Wait Times
Reducing ER wait times requires a comprehensive approach that addresses the root causes of delays. Implementing efficient triage systems, optimizing staffing models, and leveraging technology to streamline patient flow are critical strategies. Additionally, enhancing patient communication, providing clear expectations about wait times, and offering updates on the status of care can help manage patient expectations and reduce anxiety. Healthcare leaders must also prioritize staff well-being, recognizing the critical role that burnout and job satisfaction play in the ability of healthcare providers to deliver high-quality, timely care.
What is the average wait time in ERs across the US?
+The average wait time in ERs across the US is approximately 40 minutes, according to the Centers for Disease Control and Prevention (CDC).
What factors contribute to ER wait times?
+Key factors include patient volume, severity of conditions, medical staff availability, and hospital resource allocation.
How can ER wait times be reduced?
+Effective strategies include implementing efficient triage systems, optimizing staffing models, leveraging technology for patient flow, and enhancing patient communication.
In conclusion, addressing ER wait times is a complex challenge that requires a multifaceted approach. By understanding the factors that contribute to wait times, implementing evidence-based strategies to reduce them, and prioritizing patient-centered care, healthcare leaders can work towards creating more efficient and effective ER environments. This not only improves patient outcomes and satisfaction but also supports the well-being of healthcare providers and contributes to a more sustainable healthcare system.