Heart medications, also known as cardiovascular medications, are a crucial part of managing and treating various heart conditions, such as high blood pressure, coronary artery disease, heart failure, and arrhythmias. These medications work by reducing the workload on the heart, improving blood flow, and preventing further damage to the heart and blood vessels. With the rising prevalence of heart disease worldwide, the importance of heart medications cannot be overstated. According to the World Health Organization (WHO), approximately 17.9 million people die from cardiovascular diseases every year, accounting for 31% of all deaths globally.
The development and use of heart medications have undergone significant advancements over the years, with researchers continually striving to create more effective and targeted treatments. For instance, the introduction of beta blockers in the 1960s revolutionized the management of hypertension and angina, while the discovery of angiotensin-converting enzyme (ACE) inhibitors in the 1980s provided a new approach to treating heart failure. Today, there are numerous classes of heart medications available, each with its unique mechanism of action and benefits.
Key Points
- Heart medications are a crucial part of managing and treating various heart conditions, such as high blood pressure, coronary artery disease, heart failure, and arrhythmias.
- There are several classes of heart medications, including beta blockers, ACE inhibitors, diuretics, and statins, each with its unique mechanism of action and benefits.
- Heart medications can help reduce the risk of heart attack, stroke, and other cardiovascular events by improving blood flow, reducing blood pressure, and preventing further damage to the heart and blood vessels.
- Lifestyle modifications, such as a healthy diet, regular exercise, and stress management, are essential for maximizing the effectiveness of heart medications.
- Regular monitoring and follow-up with a healthcare provider are crucial for adjusting medication regimens and preventing potential side effects.
Classes of Heart Medications
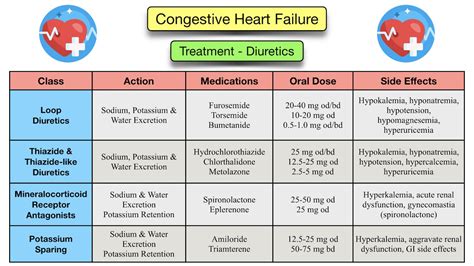
There are several classes of heart medications, each with its unique mechanism of action and benefits. Beta blockers, for example, work by slowing the heart rate and reducing the force of the heart’s contractions, thereby decreasing blood pressure and improving blood flow. ACE inhibitors, on the other hand, block the production of angiotensin II, a potent vasoconstrictor that can increase blood pressure and worsen heart failure. Other classes of heart medications include diuretics, which help remove excess fluid from the body, and statins, which lower cholesterol levels and reduce the risk of heart attack and stroke.
Angiotensin-Receptor Blockers (ARBs)
Angiotensin-receptor blockers (ARBs) are another class of heart medications that work by blocking the action of angiotensin II, a potent vasoconstrictor that can increase blood pressure and worsen heart failure. ARBs are often used in combination with other medications, such as ACE inhibitors and beta blockers, to provide additional blood pressure control and cardiovascular protection. According to a study published in the New England Journal of Medicine, the use of ARBs in patients with heart failure can reduce the risk of hospitalization and death by 15% and 11%, respectively.
| Medication Class | Mechanism of Action | Benefits |
|---|---|---|
| Beta Blockers | Slow heart rate and reduce contractility | Decrease blood pressure, improve blood flow, and reduce risk of heart attack |
| ACE Inhibitors | Block production of angiotensin II | Decrease blood pressure, improve heart function, and reduce risk of heart failure |
| Diuretics | Remove excess fluid from the body | Reduce blood pressure, improve blood flow, and decrease risk of edema |
| Statins | Lower cholesterol levels | Reduce risk of heart attack and stroke, and slow progression of atherosclerosis |
Lifestyle Modifications and Heart Health

Lifestyle modifications are essential for maximizing the effectiveness of heart medications and improving overall cardiovascular health. A healthy diet that is low in sodium, saturated fat, and added sugars, and high in fruits, vegetables, and whole grains, can help reduce blood pressure, improve blood lipid profiles, and decrease the risk of heart disease. Regular exercise, such as brisk walking, jogging, or swimming, can also help improve cardiovascular health by increasing blood flow, reducing inflammation, and improving insulin sensitivity. Additionally, stress management techniques, such as meditation, yoga, or deep breathing, can help reduce stress and anxiety, which can exacerbate heart disease.
Monitoring and Follow-up
Regular monitoring and follow-up with a healthcare provider are crucial for adjusting medication regimens and preventing potential side effects. Patients with heart disease should have regular check-ups with their healthcare provider to monitor their blood pressure, blood lipid profiles, and kidney function, and to adjust their medication regimen as needed. According to a study published in the Journal of the American College of Cardiology, regular monitoring and follow-up can reduce the risk of hospitalization and death in patients with heart failure by 25% and 18%, respectively.
What are the most common side effects of heart medications?
+The most common side effects of heart medications include dizziness, lightheadedness, fatigue, and nausea. However, these side effects are usually mild and temporary, and can be managed by adjusting the medication regimen or lifestyle modifications.
How long do I need to take heart medications?
+The duration of heart medication therapy depends on the individual patient and the specific heart condition being treated. In some cases, patients may need to take heart medications for the rest of their lives, while in other cases, medications may be discontinued after a certain period of time.
Can I stop taking my heart medications if I feel better?
+No, it is not recommended to stop taking heart medications without consulting a healthcare provider. Stopping heart medications abruptly can lead to a worsening of symptoms, increased risk of cardiovascular events, and even death.
In conclusion, heart medications are a crucial part of managing and treating various heart conditions, and can help reduce the risk of heart attack, stroke, and other cardiovascular events. By understanding the different classes of heart medications, lifestyle modifications, and monitoring and follow-up, patients with heart disease can work with their healthcare provider to develop an effective treatment plan that improves their overall cardiovascular health and quality of life.