Heparin, a widely used anticoagulant, plays a crucial role in preventing and treating thrombosis. Its application spans various medical specialties, including cardiology, surgery, and nephrology. Understanding heparin's mechanisms, benefits, and potential risks is essential for healthcare professionals to ensure safe and effective use. Here, we delve into five key tips regarding heparin, focusing on its administration, monitoring, and management of potential complications.
Key Points
- Initial Dosing and Bolus: Understanding the appropriate initial dosing and the role of bolus administration in achieving rapid anticoagulation.
- Monitoring with aPTT: The importance of regular monitoring using activated Partial Thromboplastin Time (aPTT) to adjust heparin doses and maintain therapeutic anticoagulation levels.
- Recognizing and Managing Bleeding: Early identification and management of bleeding complications, which are among the most significant risks associated with heparin therapy.
- Heparin-Induced Thrombocytopenia (HIT): Awareness of HIT, a potentially life-threatening complication, and the measures to diagnose and manage it effectively.
- Transitioning to Warfarin: Strategies for safely transitioning patients from heparin to warfarin, ensuring continuous anticoagulation without increasing the risk of thrombosis or bleeding.
Understanding Heparin Administration
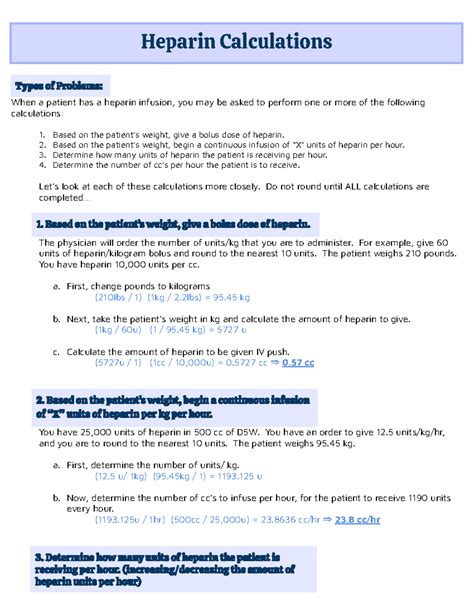
Heparin administration is a complex process that requires careful consideration of several factors, including the patient’s weight, renal function, and the presence of any bleeding risks. The initial dosing of heparin is critical and often involves a bolus dose followed by a continuous infusion. The bolus dose is typically 50-100 units/kg, and the infusion rate is adjusted based on the patient’s aPTT levels. Regular monitoring of aPTT is essential to ensure that the patient remains within the therapeutic range, thereby minimizing the risk of both thrombosis and bleeding.
Monitoring with aPTT
The therapeutic range for heparin, as measured by aPTT, is generally considered to be between 60 and 80 seconds, although this can vary slightly depending on the laboratory and the specific assay used. Frequent aPTT measurements are necessary, especially during the initial stages of heparin therapy, to ensure that the dose is appropriately adjusted. This monitoring helps in achieving and maintaining therapeutic anticoagulation levels, thus preventing both thrombotic events and bleeding complications.
| Parameter | Target Range |
|---|---|
| aPTT (seconds) | 60-80 seconds |
| Anti-Xa levels (for low molecular weight heparin) | 0.5-1.0 units/mL |
Recognizing and Managing Complications
Despite its effectiveness, heparin therapy is associated with several potential complications, the most significant of which are bleeding and heparin-induced thrombocytopenia (HIT). Bleeding complications can range from minor, such as bruising or petechiae, to life-threatening, including intracranial hemorrhage. Early recognition of bleeding is critical, and management may involve discontinuing heparin, administering protamine sulfate as an antidote, and providing supportive care as needed.
Heparin-Induced Thrombocytopenia (HIT)
HIT is a potentially life-threatening complication of heparin therapy, occurring in approximately 1-5% of patients receiving unfractionated heparin. It is characterized by a decrease in platelet count, typically occurring 5-10 days after the initiation of heparin, and is associated with a high risk of thrombosis. Early recognition of HIT, based on clinical suspicion and laboratory confirmation, is crucial. Management involves immediate discontinuation of heparin and initiation of an alternative anticoagulant, such as a direct thrombin inhibitor.
Transitioning to Warfarin
In patients requiring long-term anticoagulation, heparin is often used as a bridge until warfarin therapy is established. The transition from heparin to warfarin requires careful planning to ensure continuous anticoagulation without increasing the risk of thrombosis or bleeding. This typically involves overlapping heparin and warfarin for a period, usually until the international normalized ratio (INR) is within the therapeutic range for two consecutive days. Monitoring of INR levels is then used to adjust the warfarin dose, ensuring that the patient remains adequately anticoagulated.
What is the primary method for monitoring heparin therapy?
+The primary method for monitoring heparin therapy is through the use of activated Partial Thromboplastin Time (aPTT). This test measures the time it takes for blood to clot and is used to ensure that heparin doses are appropriately adjusted to maintain therapeutic anticoagulation levels.
How is heparin-induced thrombocytopenia (HIT) diagnosed?
+HIT is diagnosed based on a combination of clinical suspicion and laboratory confirmation. This includes a significant decrease in platelet count (typically >50% from baseline) and the presence of antibodies against the heparin-platelet factor 4 complex, which can be detected through specific assays.
What is the appropriate strategy for transitioning a patient from heparin to warfarin?
+The appropriate strategy involves overlapping heparin and warfarin therapy. Heparin is continued until the international normalized ratio (INR) is within the therapeutic range for two consecutive days, ensuring continuous anticoagulation and minimizing the risk of thrombosis or bleeding.
In conclusion, heparin is a powerful anticoagulant that requires careful management to ensure its safe and effective use. By understanding the nuances of heparin administration, monitoring, and the management of potential complications, healthcare professionals can provide high-quality care to patients requiring anticoagulation therapy. Continuous education and awareness of the latest guidelines and best practices are essential in optimizing outcomes for patients on heparin therapy.