Ibuprofen and meloxicam are two commonly prescribed nonsteroidal anti-inflammatory drugs (NSAIDs) used to treat various types of pain and inflammation. While both medications share similar mechanisms of action, they exhibit distinct differences in terms of their pharmacological properties, efficacy, and safety profiles. In this article, we will delve into the comparison of ibuprofen and meloxicam, exploring their differences, similarities, and clinical implications.
Key Points
- Ibuprofen and meloxicam are both NSAIDs with anti-inflammatory, analgesic, and antipyretic properties
- Ibuprofen has a faster onset of action, while meloxicam has a longer duration of action
- Meloxicam is more selective for COX-2 inhibition, which may reduce gastrointestinal side effects
- Ibuprofen is more commonly used for acute pain management, while meloxicam is often prescribed for chronic pain conditions
- Both medications require careful consideration of individual patient factors, such as renal function and cardiovascular risk
Pharmacological Properties and Mechanisms of Action
Ibuprofen and meloxicam belong to the same class of medications, but they differ in their chemical structures and pharmacokinetic profiles. Ibuprofen is a propionic acid derivative, while meloxicam is an enolic acid derivative. These differences influence their absorption, distribution, metabolism, and excretion (ADME) characteristics. Ibuprofen is rapidly absorbed, with peak plasma concentrations reached within 1-2 hours, whereas meloxicam has a slower absorption rate, with peak levels achieved within 4-5 hours.
COX-2 Selectivity and Gastrointestinal Safety
Meloxicam is considered a more selective COX-2 inhibitor compared to ibuprofen, which may contribute to its relatively lower risk of gastrointestinal side effects. COX-2 selectivity refers to a medication’s ability to preferentially inhibit the COX-2 enzyme, which is involved in the production of prostaglandins that promote inflammation and pain. In contrast, COX-1 is responsible for maintaining the protective lining of the stomach and intestines. By being more selective for COX-2, meloxicam may reduce the risk of gastrointestinal complications, such as ulcers and bleeding, which are common concerns with NSAID use.
| Medication | COX-2 Selectivity | Gastrointestinal Risk |
|---|---|---|
| Ibuprofen | Non-selective | Higher |
| Meloxicam | More selective | Lower |
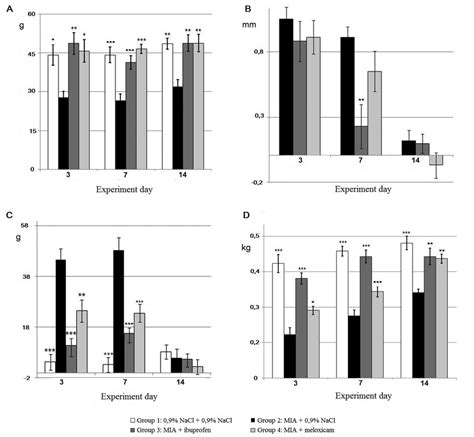
Clinical Efficacy and Indications
Both ibuprofen and meloxicam are effective for managing various types of pain and inflammation, including osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis. However, ibuprofen is often preferred for acute pain conditions, such as headaches and musculoskeletal injuries, due to its faster onset of action. In contrast, meloxicam is commonly used for chronic pain management, as its longer duration of action provides sustained relief.
Dosing and Administration
The dosing and administration of ibuprofen and meloxicam vary depending on the specific indication and patient population. Ibuprofen is typically administered in doses of 200-400 mg every 4-6 hours, while meloxicam is usually given in doses of 7.5-15 mg once daily. It is essential to follow the recommended dosing guidelines and adjust the medication regimen according to individual patient needs and response.
What are the primary differences between ibuprofen and meloxicam?
+The primary differences between ibuprofen and meloxicam lie in their pharmacological properties, mechanisms of action, and clinical indications. Ibuprofen has a faster onset of action, while meloxicam has a longer duration of action. Meloxicam is also more selective for COX-2 inhibition, which may reduce gastrointestinal side effects.
Which medication is more suitable for chronic pain management?
+Meloxicam is often preferred for chronic pain management due to its longer duration of action, which provides sustained relief. However, the choice between ibuprofen and meloxicam ultimately depends on individual patient factors, such as renal function, cardiovascular risk, and gastrointestinal health.
What are the potential gastrointestinal risks associated with NSAID use?
+The potential gastrointestinal risks associated with NSAID use include ulcers, bleeding, and perforation of the stomach and intestines. These risks can be mitigated by using medications with higher COX-2 selectivity, such as meloxicam, and by implementing strategies to reduce gastrointestinal toxicity, such as concomitant use of proton pump inhibitors.
In conclusion, ibuprofen and meloxicam are both effective NSAIDs with distinct differences in their pharmacological properties, mechanisms of action, and clinical indications. While ibuprofen is often preferred for acute pain conditions, meloxicam is commonly used for chronic pain management. Clinicians should carefully consider individual patient factors, such as renal function, cardiovascular risk, and gastrointestinal health, when choosing between these medications. By understanding the nuances of ibuprofen and meloxicam, healthcare professionals can provide optimal care for patients requiring NSAID therapy.