The realm of infectious disease health science is a multifaceted and dynamic field, continually evolving with new discoveries and advancements in medical research. As a domain-specific expert with a background in epidemiology and microbiology, it is essential to acknowledge the significance of understanding the intricacies of infectious diseases, from their molecular mechanisms to their impact on global health. The World Health Organization (WHO) estimates that infectious diseases account for approximately 16.5% of all deaths worldwide, with the majority being attributed to respiratory infections, diarrheal diseases, and malaria. These statistics underscore the need for comprehensive insights into the causes, prevention, and treatment of infectious diseases, which can inform evidence-based public health strategies and policies.
Key Points
- The molecular mechanisms of infectious diseases involve complex interactions between pathogens and host cells, necessitating a deep understanding of microbiology and immunology.
- Epidemiological studies have identified key risk factors for infectious disease transmission, including poor sanitation, inadequate healthcare infrastructure, and climate change.
- Vaccination remains a cornerstone of infectious disease prevention, with vaccines estimated to prevent approximately 10 million deaths worldwide between 2010 and 2015.
- Antimicrobial resistance (AMR) poses a significant threat to global health, with the WHO estimating that AMR is responsible for approximately 700,000 deaths annually.
- Integrated disease surveillance and response systems are critical for detecting and responding to infectious disease outbreaks, requiring collaboration between healthcare providers, laboratories, and public health officials.
Understanding the Molecular Mechanisms of Infectious Diseases
The molecular mechanisms underlying infectious diseases are intricate and involve a complex interplay between pathogens and host cells. Pathogens, such as bacteria, viruses, and parasites, have evolved various strategies to infect and replicate within host cells, often exploiting host cellular processes to facilitate their survival and dissemination. For instance, Streptococcus pneumoniae, a common cause of pneumonia, can adhere to and invade host epithelial cells, triggering an inflammatory response that contributes to disease pathogenesis. Elucidating these molecular mechanisms is essential for developing effective therapeutic interventions and vaccines, which can target specific pathways or components of the host-pathogen interaction.
Epidemiological Insights into Infectious Disease Transmission
Epidemiological studies have provided valuable insights into the risk factors and transmission dynamics of infectious diseases. Respiratory infections, such as influenza and tuberculosis, are often spread through respiratory droplets, while diarrheal diseases, like cholera and rotavirus, are frequently transmitted through contaminated food and water. Climate change has also been implicated in the emergence and spread of infectious diseases, with rising temperatures and altered precipitation patterns facilitating the proliferation of disease vectors, such as mosquitoes and ticks. Understanding these epidemiological factors is crucial for developing targeted public health interventions and mitigating the impact of infectious diseases on vulnerable populations.
| Infectious Disease | Transmission Route | Global Burden |
|---|---|---|
| Influenza | Respiratory droplets | 3-5 million cases annually |
| Tuberculosis | Respiratory droplets | 10 million cases annually |
| Cholera | Contaminated food and water | 1.3-4.0 million cases annually |
| Rotavirus | Fecal-oral route | 111 million cases annually |
Addressing the Challenge of Antimicrobial Resistance
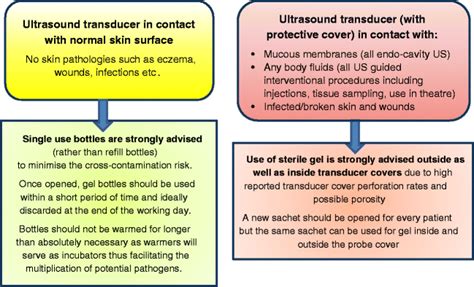
Antimicrobial resistance (AMR) poses a significant threat to global health, with the WHO estimating that AMR is responsible for approximately 700,000 deaths annually. The overuse and misuse of antibiotics have contributed to the emergence and spread of AMR, highlighting the need for stewardship programs that promote responsible antibiotic use and monitor resistance patterns. Alternatives to antibiotics, such as bacteriophage therapy and antimicrobial peptides, are also being explored, offering potential solutions to the AMR crisis. Furthermore, infection prevention and control measures, such as hand hygiene and proper wound care, can help mitigate the spread of AMR pathogens in healthcare settings.
Integrated Disease Surveillance and Response Systems
Integrated disease surveillance and response systems are critical for detecting and responding to infectious disease outbreaks, requiring collaboration between healthcare providers, laboratories, and public health officials. Syndromic surveillance systems, which monitor patient symptoms and laboratory results, can facilitate early detection of outbreaks, while genomic sequencing can provide valuable insights into the molecular epidemiology of infectious diseases. The implementation of these systems is essential for preventing and controlling infectious disease outbreaks, ultimately protecting public health and preventing unnecessary morbidity and mortality.
What are the primary risk factors for infectious disease transmission?
+The primary risk factors for infectious disease transmission include poor sanitation, inadequate healthcare infrastructure, and climate change. These factors can facilitate the spread of infectious diseases, particularly in vulnerable populations.
How can antimicrobial resistance be addressed?
+Antimicrobial resistance can be addressed through stewardship programs that promote responsible antibiotic use, monitor resistance patterns, and develop alternatives to antibiotics. Infection prevention and control measures, such as hand hygiene and proper wound care, can also help mitigate the spread of AMR pathogens.
What is the role of integrated disease surveillance and response systems in preventing and controlling infectious disease outbreaks?
+Integrated disease surveillance and response systems play a critical role in detecting and responding to infectious disease outbreaks, facilitating early detection, and preventing unnecessary morbidity and mortality. These systems require collaboration between healthcare providers, laboratories, and public health officials.
In conclusion, the realm of infectious disease health science is complex and multifaceted, requiring a deep understanding of the molecular mechanisms underlying infectious diseases, epidemiological insights into transmission dynamics, and the development of effective public health strategies and policies. As a domain-specific expert, it is essential to stay abreast of the latest research and advancements in this field, integrating new insights into evidence-based public health approaches and promoting a comprehensive understanding of infectious diseases and their impact on global health.