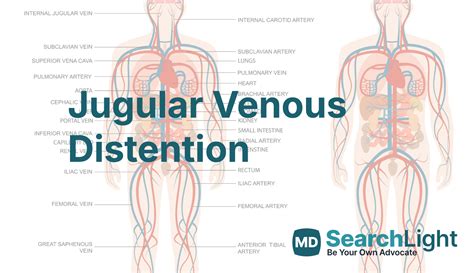
The medical field is replete with abbreviations, each serving as a shorthand to convey complex information efficiently. One such abbreviation is JVD, which stands for Jugular Venous Distension. JVD is a significant clinical sign that indicates an increase in the jugular venous pressure (JVP), reflecting the pressure inside the jugular veins. The jugular veins are major blood vessels that return deoxygenated blood from the head, face, and neck to the heart. Understanding JVD is crucial for diagnosing and managing various cardiovascular and respiratory conditions.
Understanding Jugular Venous Distension (JVD)
JVD is observed as a swelling of the jugular vein, which can be seen as a bulge in the neck. It is a vital sign that healthcare providers check during physical examinations. The Jugular Venous Pressure (JVP) is the pressure within the jugular vein and is used as an indicator of the pressure in the right atrium, one of the chambers of the heart. An elevated JVP, manifested as JVD, can be due to various reasons including heart failure, fluid overload, and other conditions that increase the pressure within the thoracic cavity.
Causes and Implications of JVD
The presence of JVD can imply several underlying conditions that need prompt medical attention. Heart failure is one of the primary causes, where the heart’s inability to pump blood efficiently leads to a backlog of blood in the veins, causing them to distend. Other causes include constrictive pericarditis, where the sac surrounding the heart becomes scarred and contracted, limiting the heart’s ability to expand and fill properly, and cardiac tamponade, a condition where fluid accumulates in the pericardial space, compressing the heart and impeding its function. JVD can also be seen in cases of pulmonary hypertension, where high blood pressure in the arteries of the lungs puts strain on the right side of the heart, and in severe respiratory conditions such as chronic obstructive pulmonary disease (COPD) and pneumonia, which can increase the pressure in the thoracic cavity.
| Condition | Description |
|---|---|
| Heart Failure | Inability of the heart to pump enough blood to meet the body's needs |
| Constrictive Pericarditis | Scarring and contraction of the pericardium, restricting heart expansion |
| Cardiac Tamponade | Fluid accumulation in the pericardial space, compressing the heart |
| Pulmonary Hypertension | High blood pressure in the lungs' arteries, straining the right heart |
| Severe Respiratory Conditions | Conditions like COPD and pneumonia that increase thoracic pressure |
Key Points
- JVD stands for Jugular Venous Distension, a clinical sign of increased jugular venous pressure.
- It is a critical indicator of the pressure in the right atrium and can signal various cardiovascular and respiratory conditions.
- Causes of JVD include heart failure, fluid overload, constrictive pericarditis, cardiac tamponade, pulmonary hypertension, and severe respiratory diseases.
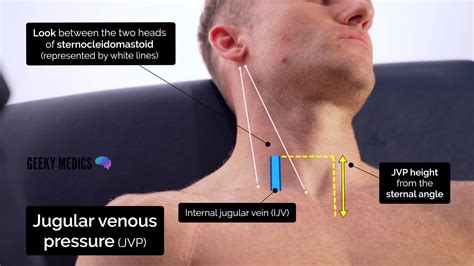
- The assessment of JVD involves careful observation and palpation of the jugular vein, with the patient positioned at a 45-degree angle.
- Understanding the JVP waveform can provide insights into the heart's function and help in diagnosing potential problems.
In clinical practice, the evaluation of JVD is part of a comprehensive assessment that includes history taking, physical examination, and diagnostic tests such as echocardiography and chest X-rays. Managing conditions associated with JVD often requires a multidisciplinary approach, including medication to reduce fluid overload and improve heart function, and in some cases, surgical interventions to address underlying causes. The significance of JVD underscores the importance of regular health check-ups and prompt medical evaluation for symptoms such as shortness of breath, fatigue, and swelling in the legs and feet, which can be indicative of underlying heart or lung disease.
What does JVD indicate in a medical context?
+JVD, or Jugular Venous Distension, indicates an increase in the pressure within the jugular veins, which can signal various heart and lung conditions, including heart failure, fluid overload, and severe respiratory diseases.
How is JVD diagnosed?
+Diagnosis of JVD involves physical examination, where the healthcare provider looks for signs of jugular vein distension and measures the jugular venous pressure. Additional diagnostic tests such as echocardiography and chest X-rays may be conducted to determine the underlying cause.
What are the common causes of JVD?
+Common causes of JVD include heart failure, constrictive pericarditis, cardiac tamponade, pulmonary hypertension, and severe respiratory conditions like COPD and pneumonia. Each of these conditions affects the heart's ability to function properly, leading to increased pressure in the jugular veins.
How is JVD managed?
+Management of JVD depends on the underlying cause and may involve medication to reduce fluid overload and improve heart function, lifestyle modifications, and in some cases, surgical intervention to address the root cause of the condition.
Why is early detection of JVD important?
+Early detection of JVD is crucial because it allows for the prompt identification and management of underlying conditions that could lead to serious complications if left untreated. Regular health check-ups and awareness of symptoms such as shortness of breath and leg swelling can facilitate early detection and intervention.
In conclusion, JVD is a critical clinical sign that necessitates a thorough evaluation and understanding of its causes and implications. By recognizing the significance of JVD and adopting a proactive approach to health, individuals can work closely with healthcare providers to manage associated conditions effectively and improve outcomes.