Medicaid, a joint federal-state program, provides health coverage to millions of Americans, including low-income individuals, families, and children, as well as pregnant women, elderly adults, and people with disabilities. One of the key benefits of Medicaid is its coverage of prescription medications, which is crucial for managing chronic conditions, treating acute illnesses, and improving overall health outcomes. The list of medications covered by Medicaid varies from state to state, as each state's Medicaid program has its own formulary, or list of covered drugs.
Understanding Medicaid’s Drug Coverage
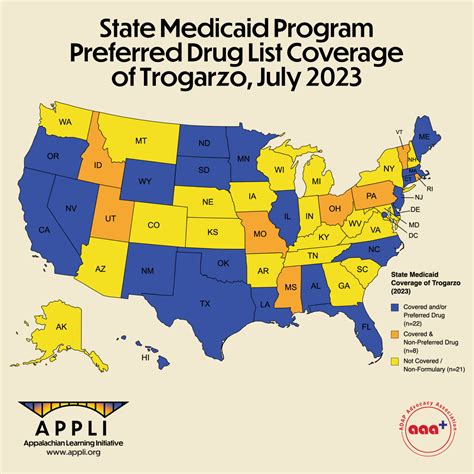
Medicaid’s drug coverage is designed to provide access to necessary medications while also managing costs and ensuring the most effective treatments are used. The program covers a wide range of medications, including brand-name and generic drugs, across various therapeutic categories. However, the specific medications covered can differ significantly between states due to differences in state Medicaid policies, formulary management, and negotiated prices with pharmaceutical manufacturers.
Factors Influencing Medicaid Drug Coverage
Several factors influence which medications are covered by Medicaid. These include the drug’s therapeutic class, its effectiveness compared to other available treatments, the presence of generic alternatives, and the drug’s cost. Medicaid programs also consider recommendations from professional medical societies, clinical guidelines, and evidence-based medicine when making coverage decisions.
| Medication Category | Examples of Covered Medications |
|---|---|
| Antibiotics | Azithromycin, Amoxicillin, Cephalexin |
| Antihypertensives | Lisinopril, Atenolol, Metoprolol |
| Antidepressants | Fluoxetine, Sertraline, Bupropion |
| Asthma Medications | Albuterol, Fluticasone, Salmeterol |
| Diabetes Medications | Metformin, Glipizide, Insulin |
Key Points

Key Points
- Medicaid covers a wide range of prescription medications, but the specific list varies by state.
- The coverage decision is influenced by the drug’s efficacy, cost, and availability of generic alternatives.
- States manage their Medicaid formularies to balance access to necessary medications with cost management.
- Prior authorization, step therapy, and quantity limits are common management tools used by Medicaid programs.
- Patients and healthcare providers should consult the state’s Medicaid website or contact the program directly for the most current and accurate information on covered medications.
Accessing Medicaid Drug Coverage Information
To find out which medications are covered by Medicaid in a specific state, individuals can visit the state’s Medicaid website or contact the Medicaid program directly. Healthcare providers can also access this information through the state’s Medicaid provider portal or by contacting the program’s pharmacy services department. Additionally, the Centers for Medicare & Medicaid Services (CMS) provides resources and tools to help states manage their Medicaid programs, including guidance on drug coverage and reimbursement.
Managing Medicaid Drug Benefits
Effective management of Medicaid drug benefits involves a collaborative effort between state Medicaid agencies, healthcare providers, patients, and pharmaceutical manufacturers. This includes ongoing review and update of formularies to ensure they reflect the latest clinical evidence and treatment guidelines, as well as efforts to control costs and improve patient access to necessary medications. By balancing these goals, Medicaid can provide comprehensive and cost-effective coverage of prescription medications to its beneficiaries.
How do I find out which medications are covered by Medicaid in my state?
+To find out which medications are covered, you can visit your state's Medicaid website, contact the Medicaid program directly, or ask your healthcare provider for assistance. They can guide you through the process and provide the most current information on covered medications.
Can Medicaid coverage of medications change?
+Yes, Medicaid coverage of medications can change over time. States regularly review and update their formularies to reflect new clinical evidence, changes in drug pricing, and the availability of generic alternatives. It's essential to stay informed through your state's Medicaid program or healthcare provider.
How does Medicaid determine which medications to cover?
+Medicaid determines which medications to cover based on their therapeutic effectiveness, safety, and cost. The decision-making process involves consideration of clinical guidelines, recommendations from professional medical societies, and input from pharmacists and physicians. The goal is to provide access to necessary and effective treatments while managing program costs.
In conclusion, Medicaid’s coverage of prescription medications is a critical component of the program, aiming to provide necessary treatments to its beneficiaries while managing costs. Understanding the factors that influence drug coverage and knowing how to access information on covered medications can help individuals navigate the system more effectively. As healthcare needs and treatment options evolve, ongoing collaboration and adaptation are necessary to ensure that Medicaid’s drug benefits continue to meet the needs of its diverse population.