Medicaid, a joint federal and state program, provides health coverage to millions of Americans, including low-income adults, children, pregnant women, elderly adults, and people with disabilities. One of the essential aspects of oral health care that Medicaid covers is orthodontic treatment, including braces, for eligible individuals, particularly children and adolescents. The coverage and eligibility for Medicaid braces vary significantly from state to state, reflecting the diverse health care needs and policies across different regions.
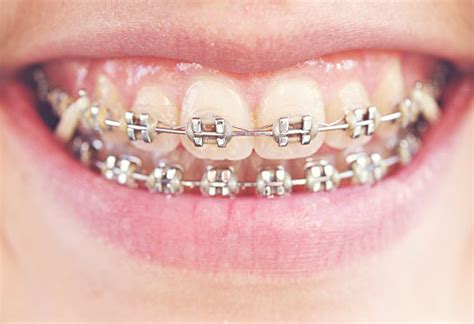
The primary goal of Medicaid's orthodontic coverage is to ensure that beneficiaries, especially children, have access to necessary dental care to correct issues that could lead to more severe health problems if left untreated. Orthodontic problems, such as malocclusions (bad bites), can affect not only the aesthetic appeal of one's smile but also overall oral health, speech, and self-esteem. Braces are a common treatment option for these issues, using brackets, wires, and other appliances to apply gentle pressure to teeth, guiding them into their proper positions over time.
Key Points
- Medicaid coverage for orthodontic braces varies by state, with each state having its own guidelines and eligibility criteria.
- The program primarily focuses on covering orthodontic treatments for children and adolescents, with coverage for adults being less common and usually limited to severe cases.
- To qualify for Medicaid-covered orthodontic care, individuals must meet specific medical necessity criteria, which often include the presence of severe orthodontic issues that impact oral health and function.
- The application and approval process for Medicaid orthodontic coverage involves a comprehensive evaluation by an orthodontist, submission of detailed treatment plans, and review by state Medicaid agencies to determine medical necessity.
- Given the variability in coverage and the specific requirements that must be met, it's essential for families and individuals to consult with their state's Medicaid program and orthodontic specialists to understand the eligibility criteria and application process.
Eligibility and Coverage

The eligibility for Medicaid-covered braces is contingent upon meeting the medical necessity criteria as defined by each state. Generally, these criteria include the presence of significant orthodontic issues that are likely to cause oral health problems, such as difficulty chewing, speaking, or maintaining oral hygiene, if left untreated. States often use indexes like the Handicapping Labio-Lingual Deviation (HLD) index or the Index of Orthodontic Treatment Need (IOTN) to assess the severity of malocclusions and determine the need for treatment.
While the primary focus of Medicaid's orthodontic coverage is on children, some states may also cover orthodontic care for adults under certain circumstances, such as when orthodontic treatment is necessary to address a medical condition or to facilitate other dental treatments like denture placement. However, such coverage is less common and usually requires a more rigorous approval process to demonstrate medical necessity.
Application and Approval Process
The process of applying for and receiving approval for Medicaid-covered orthodontic braces involves several steps. Initially, an individual must be eligible for Medicaid and then undergo an evaluation by an orthodontist to assess the need for orthodontic treatment. If the orthodontist determines that treatment is necessary, a detailed treatment plan, including records and photographs, is prepared and submitted to the state Medicaid agency for review.
The Medicaid agency then assesses the treatment plan against the state's medical necessity criteria to determine if the treatment is covered. This review process can be lengthy, and not all applications are approved. In cases where approval is denied, families may have the option to appeal the decision, providing additional information or seeking a second opinion to support the medical necessity of the treatment.
| State | Coverage Details |
|---|---|
| California | Covers orthodontic care for children with severe malocclusions, using the HLD index for assessment. |
| New York | Provides coverage for orthodontic treatments for children and adolescents, with a focus on cases that involve significant oral health risks. |
| Texas | Covers orthodontic care for children, emphasizing the treatment of severe orthodontic issues that impact oral function and health. |

Challenges and Considerations

Despite the importance of orthodontic care and the coverage provided by Medicaid, there are challenges and considerations that families and individuals must navigate. One of the primary concerns is the variability in coverage from state to state, which can lead to confusion and disparities in access to care. Additionally, the application and approval process can be complex and time-consuming, potentially delaying the initiation of necessary treatment.
Another significant challenge is the limited availability of orthodontists who participate in Medicaid, particularly in rural and underserved areas. This can result in barriers to access, including longer wait times for appointments and the need to travel greater distances to receive care. Addressing these challenges requires a multifaceted approach, including education and outreach to increase awareness about Medicaid coverage for orthodontic care, expansion of the provider network, and simplification of the application and approval process.
Future Directions and Implications
Looking forward, it is essential to continue assessing and refining the Medicaid program’s approach to covering orthodontic care. This includes reviewing the medical necessity criteria to ensure they are up-to-date and reflect the current understanding of orthodontic needs and treatments. Moreover, efforts to expand access to care, particularly for underserved populations, and to streamline the application process can help in ensuring that more individuals receive the orthodontic treatments they need.
The implications of Medicaid's coverage of orthodontic braces extend beyond individual oral health outcomes, influencing overall well-being, self-esteem, and quality of life. By providing access to necessary orthodontic care, Medicaid plays a critical role in promoting health equity and addressing the social determinants of health that affect disadvantaged populations. As such, continued support and improvement of Medicaid's orthodontic coverage are vital for advancing the health and welfare of its beneficiaries.
How do I apply for Medicaid-covered orthodontic braces?
+To apply, you first need to be eligible for Medicaid. Then, consult with an orthodontist who participates in Medicaid to undergo an evaluation. If the orthodontist recommends treatment, they will prepare a treatment plan to submit to your state's Medicaid agency for review and approval.
What are the medical necessity criteria for Medicaid-covered orthodontic care?
+The criteria vary by state but often include the presence of severe malocclusions that are likely to cause oral health problems if left untreated. States may use specific indexes, such as the HLD or IOTN, to assess the severity of orthodontic issues.
Can adults receive Medicaid coverage for orthodontic braces?
+While less common, some states may cover orthodontic care for adults under specific circumstances, such as when treatment is necessary to address a medical condition. The eligibility criteria and application process for adults are typically more stringent than for children and adolescents.
In conclusion, Medicaid plays a vital role in ensuring that eligible individuals, particularly children and adolescents, have access to necessary orthodontic care, including braces. Understanding the eligibility criteria, application process, and the variability in coverage across states is essential for navigating the system and securing the care needed. As the healthcare landscape continues to evolve, the importance of Medicaid’s orthodontic coverage will only continue to grow, underscoring the need for ongoing assessment, improvement, and support of this critical aspect of oral health care.