Medicaid provider enrollment is a critical process that enables healthcare professionals and organizations to participate in the Medicaid program, thereby allowing them to provide essential medical services to millions of low-income individuals and families across the United States. The enrollment process involves a series of steps and requirements that vary by state, but the overall goal remains the same: to ensure that providers meet the necessary standards to deliver high-quality, cost-effective care to Medicaid beneficiaries. In this article, we will delve into the intricacies of Medicaid provider enrollment, exploring the key components, challenges, and best practices associated with this complex process.
Key Points
- Medicaid provider enrollment is a state-specific process with varying requirements and regulations
- Providers must meet certain standards, including licensure, certification, and accreditation, to participate in the Medicaid program
- The enrollment process typically involves an application, screening, and verification of credentials
- Providers must also comply with federal and state regulations, such as the Affordable Care Act and the Health Insurance Portability and Accountability Act (HIPAA)
- Effective communication and collaboration between providers, state agencies, and Medicaid managed care organizations are essential for successful enrollment and participation in the program
Medicaid Provider Enrollment Process
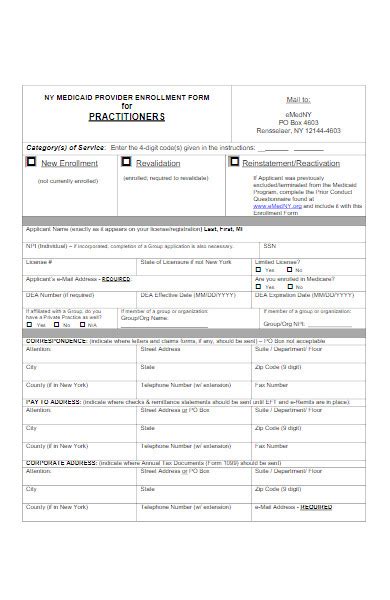
The Medicaid provider enrollment process typically begins with an application, which must be submitted to the state’s Medicaid agency or a designated enrollment vendor. The application requires providers to furnish detailed information about their practice, including their name, address, contact information, and credentials. Providers must also disclose any affiliations with other healthcare organizations or individuals, as well as any history of sanctions, suspensions, or revocations of their medical license or certification.
Following the submission of the application, the state's Medicaid agency or enrollment vendor conducts a thorough screening and verification of the provider's credentials. This includes checking the provider's licensure, certification, and accreditation status, as well as verifying their identity and credentials through various databases, such as the National Practitioner Data Bank (NPDB) and the Medicare Enrollment Database.
Requirements for Medicaid Provider Enrollment
To participate in the Medicaid program, providers must meet certain standards and requirements, which may vary by state. These requirements typically include:
- Licensure: Providers must be licensed to practice in the state where they intend to provide Medicaid services
- Certification: Providers must be certified by a recognized accrediting organization, such as the Joint Commission or the Accreditation Association for Ambulatory Health Care (AAAHC)
- Accreditation: Providers must be accredited by a recognized accrediting organization, such as the Joint Commission or the American Osteopathic Association (AOA)
- Credentialing: Providers must undergo a credentialing process, which involves verifying their education, training, and experience
In addition to these requirements, providers must also comply with federal and state regulations, such as the Affordable Care Act and the Health Insurance Portability and Accountability Act (HIPAA). These regulations govern various aspects of healthcare, including patient privacy, billing, and reimbursement.
| State | Medicaid Agency | Enrollment Vendor |
|---|---|---|
| New York | New York State Department of Health | Change Healthcare |
| California | California Department of Health Care Services | Conduent |
| Texas | Texas Health and Human Services Commission | DXC Technology |
Challenges and Best Practices in Medicaid Provider Enrollment
Despite the importance of Medicaid provider enrollment, the process is often plagued by challenges and inefficiencies. One of the most significant challenges is the complexity of the enrollment process itself, which can be time-consuming and frustrating for providers. Additionally, the lack of standardization across states can create confusion and difficulties for providers who practice in multiple states.
To overcome these challenges, providers can employ several best practices, including:
- Ensuring that all necessary documentation is complete and accurate before submitting the application
- Verifying the state's Medicaid agency or enrollment vendor's requirements and regulations
- Establishing open and effective communication with the state's Medicaid agency or enrollment vendor
- Utilizing technology, such as online portals and electronic signature tools, to streamline the enrollment process
By following these best practices and staying informed about state-specific requirements and regulations, providers can navigate the Medicaid provider enrollment process more efficiently and effectively, ultimately ensuring that they can provide high-quality care to Medicaid beneficiaries.
What is the purpose of Medicaid provider enrollment?
+The purpose of Medicaid provider enrollment is to ensure that healthcare professionals and organizations meet the necessary standards to deliver high-quality, cost-effective care to Medicaid beneficiaries.
What are the requirements for Medicaid provider enrollment?
+The requirements for Medicaid provider enrollment vary by state, but typically include licensure, certification, accreditation, and credentialing.
How long does the Medicaid provider enrollment process take?
+The length of time it takes to complete the Medicaid provider enrollment process varies by state, but can range from several weeks to several months.
As the Medicaid program continues to evolve and expand, the importance of efficient and effective provider enrollment processes will only continue to grow. By understanding the complexities and challenges associated with Medicaid provider enrollment, providers and state agencies can work together to streamline the process, reduce administrative burdens, and ultimately improve the quality and accessibility of care for Medicaid beneficiaries.