Medicaid vision coverage is a crucial aspect of healthcare for low-income individuals and families, providing essential eye care services to prevent and treat vision problems. As a vital component of the Medicaid program, vision coverage ensures that beneficiaries have access to necessary care, including routine eye exams, corrective lenses, and treatment for eye diseases. With the Medicaid program serving over 72 million people in the United States, understanding the scope and limitations of Medicaid vision coverage is essential for healthcare providers, policymakers, and beneficiaries alike.
The history of Medicaid vision coverage dates back to the inception of the Medicaid program in 1965, with the initial focus on providing basic medical services to low-income individuals. Over time, the program has evolved to include a range of vision services, recognizing the critical importance of eye health in overall well-being. Today, Medicaid vision coverage varies by state, with some states offering more comprehensive coverage than others. According to the Centers for Medicare and Medicaid Services (CMS), all states are required to provide some level of vision coverage to children under the age of 21, as mandated by the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program.
Key Points
- Medicaid vision coverage provides essential eye care services to low-income individuals and families
- Vision coverage varies by state, with some states offering more comprehensive coverage than others
- All states are required to provide some level of vision coverage to children under the age of 21
- Medicaid vision coverage includes routine eye exams, corrective lenses, and treatment for eye diseases
- The scope and limitations of Medicaid vision coverage can impact healthcare outcomes and access to care
Vision Services Covered by Medicaid
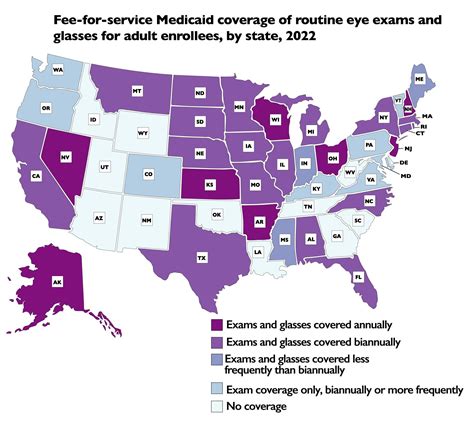
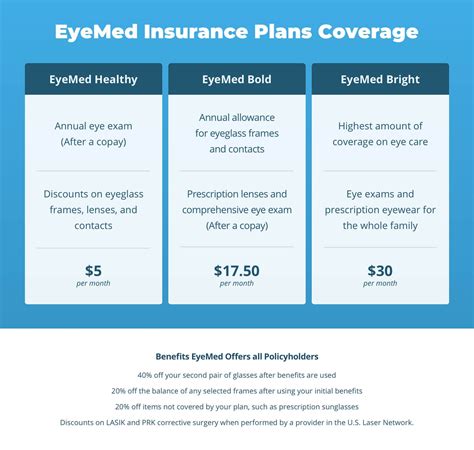
Medicaid vision coverage typically includes a range of services, such as routine eye exams, corrective lenses (e.g., glasses, contact lenses), and treatment for eye diseases (e.g., cataracts, glaucoma). Some states may also cover additional services, such as vision therapy, low vision aids, and eye prosthetics. The specific services covered and the frequency of coverage can vary significantly depending on the state and the individual’s eligibility category. For example, a study by the Kaiser Family Foundation found that 35 states and the District of Columbia provide coverage for adult vision services, while 15 states do not.
Vision Coverage for Children
As mandated by the EPSDT program, all states are required to provide comprehensive vision coverage to children under the age of 21. This coverage includes routine eye exams, corrective lenses, and treatment for eye diseases, as well as vision therapy and other specialized services. The EPSDT program ensures that children receive necessary vision care to prevent and treat vision problems, which can have a significant impact on their educational and social development. According to the American Academy of Pediatrics, early detection and treatment of vision problems can improve academic performance, reduce the risk of vision loss, and enhance overall quality of life.
| State | Vision Coverage for Adults | Vision Coverage for Children |
|---|---|---|
| California | Covered | Covered (EPSDT) |
| New York | Covered | Covered (EPSDT) |
| Texas | Not Covered | Covered (EPSDT) |
| Florida | Covered | Covered (EPSDT) |
Challenges and Limitations of Medicaid Vision Coverage

Despite the importance of Medicaid vision coverage, there are several challenges and limitations to the program. One of the primary challenges is the variability in coverage across states, which can lead to disparities in access to care. Additionally, the program’s focus on basic medical services can result in limited coverage for specialized vision services, such as low vision aids and eye prosthetics. Furthermore, the program’s reimbursement rates can be low, which can discourage healthcare providers from participating in the program. According to a report by the National Association of Community Health Centers, the reimbursement rate for Medicaid services can be as low as 50% of the cost of providing care.
Improving Medicaid Vision Coverage
To improve Medicaid vision coverage, it’s essential to address the challenges and limitations of the program. This can include increasing reimbursement rates, expanding coverage to include specialized vision services, and promoting awareness of the program among healthcare providers and beneficiaries. Additionally, states can work to streamline the enrollment process and reduce administrative barriers to care. By taking these steps, Medicaid vision coverage can be strengthened, ensuring that low-income individuals and families have access to necessary vision care. As noted by the National Eye Institute, improving access to vision care can have a significant impact on overall health and well-being, reducing the risk of falls, injuries, and other health problems.
What vision services are covered by Medicaid?
+Medicaid vision coverage typically includes routine eye exams, corrective lenses, and treatment for eye diseases. Some states may also cover additional services, such as vision therapy, low vision aids, and eye prosthetics.
Do all states provide vision coverage to adults?
+No, not all states provide vision coverage to adults. While some states provide comprehensive coverage, others may only provide limited coverage or none at all.
How can I find out what vision services are covered by Medicaid in my state?
+You can contact your state's Medicaid agency or visit their website to find out what vision services are covered by Medicaid in your state. You can also ask your healthcare provider or a patient advocate for assistance.
In conclusion, Medicaid vision coverage is a vital component of the Medicaid program, providing essential eye care services to low-income individuals and families. While the program has its challenges and limitations, it’s essential to recognize the importance of vision care in overall health and well-being. By understanding the scope and limitations of Medicaid vision coverage, healthcare providers and policymakers can work to improve the program, ensuring that beneficiaries receive necessary vision care. As the healthcare landscape continues to evolve, it’s crucial to prioritize Medicaid vision coverage, promoting health equity and reducing disparities in access to care.