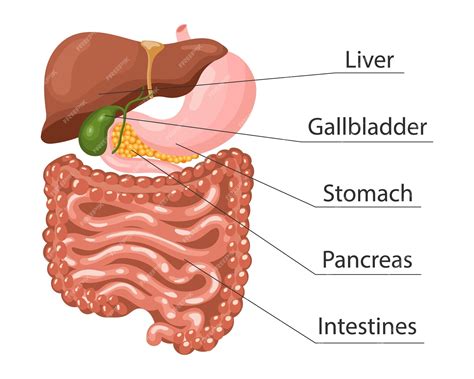
The pancreas is a vital organ located in the abdominal cavity, responsible for producing hormones and enzymes that aid in digestion and regulate blood sugar levels. Despite its crucial role, the pancreas can be affected by various medical conditions, some of which can be life-threatening if left untreated. In this article, we will delve into the different medical conditions that can affect the pancreas, their causes, symptoms, diagnosis, and treatment options.
Key Points
- The pancreas is a vital organ that produces hormones and enzymes for digestion and blood sugar regulation.
- Acute pancreatitis is a sudden and severe inflammation of the pancreas, often caused by gallstones or excessive alcohol consumption.
- Chronic pancreatitis is a long-term inflammation of the pancreas, leading to scarring and permanent damage.
- Diabetes mellitus is a group of metabolic disorders characterized by high blood sugar levels, often caused by pancreatic dysfunction.
- Pancreatic cancer is a rare but deadly disease, with a 5-year survival rate of around 9% for patients diagnosed with pancreatic adenocarcinoma.
Acute Pancreatitis
Acute pancreatitis is a sudden and severe inflammation of the pancreas, which can be caused by a variety of factors, including gallstones, excessive alcohol consumption, certain medications, and high levels of triglycerides in the blood. The symptoms of acute pancreatitis can vary in severity, but common signs include severe abdominal pain, nausea, vomiting, and fever. If left untreated, acute pancreatitis can lead to serious complications, such as organ failure, infection, and even death.
Causes and Risk Factors
The exact cause of acute pancreatitis can be difficult to determine, but certain risk factors can increase the likelihood of developing the condition. These risk factors include a history of gallstones, excessive alcohol consumption, obesity, and a family history of pancreatitis. Additionally, certain medications, such as corticosteroids and certain antibiotics, can increase the risk of developing acute pancreatitis.
| Causes of Acute Pancreatitis | Percentage of Cases |
|---|---|
| Gallstones | 40-50% |
| Excessive alcohol consumption | 20-30% |
| Idiopathic | 10-20% |
| Other causes (medications, infections, etc.) | 10-20% |

Chronic Pancreatitis
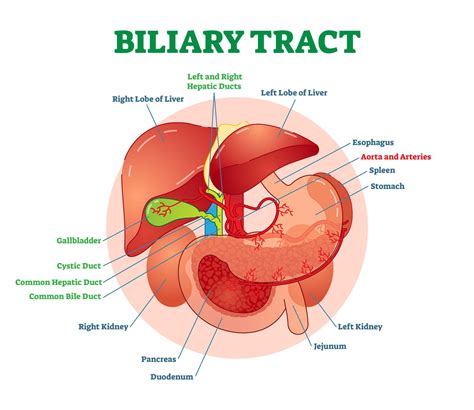
Chronic pancreatitis is a long-term inflammation of the pancreas, which can lead to scarring and permanent damage. The symptoms of chronic pancreatitis can be similar to those of acute pancreatitis, but may also include weight loss, diarrhea, and abdominal pain that worsens after eating. Chronic pancreatitis can be caused by a variety of factors, including excessive alcohol consumption, genetic disorders, and certain medications.
Diagnosis and Treatment
Diagnosing chronic pancreatitis can be challenging, as the symptoms can be similar to those of other conditions. Imaging tests, such as CT scans and MRI, can help diagnose chronic pancreatitis, as well as blood tests to measure pancreatic enzyme levels. Treatment for chronic pancreatitis typically involves managing symptoms, such as pain and diarrhea, and addressing underlying causes, such as alcohol cessation or medication adjustment.
Diabetes Mellitus
Diabetes mellitus is a group of metabolic disorders characterized by high blood sugar levels, often caused by pancreatic dysfunction. There are several types of diabetes, including type 1, type 2, and gestational diabetes. Type 1 diabetes is an autoimmune disease, in which the immune system attacks the insulin-producing beta cells in the pancreas, while type 2 diabetes is often caused by insulin resistance and impaired insulin secretion.
Treatment and Management
Treatment for diabetes typically involves managing blood sugar levels through a combination of medication, diet, and lifestyle changes. For type 1 diabetes, insulin therapy is necessary to replace the insulin that the pancreas is no longer producing. For type 2 diabetes, treatment may involve oral medications, such as metformin, and lifestyle changes, such as weight loss and increased physical activity.
Pancreatic Cancer
Pancreatic cancer is a rare but deadly disease, with a 5-year survival rate of around 9% for patients diagnosed with pancreatic adenocarcinoma. The symptoms of pancreatic cancer can be non-specific, but may include abdominal pain, weight loss, and jaundice. Risk factors for pancreatic cancer include a family history of the disease, smoking, and certain genetic disorders, such as BRCA2.
Diagnosis and Treatment
Diagnosing pancreatic cancer can be challenging, as the symptoms can be similar to those of other conditions. Imaging tests, such as CT scans and MRI, can help diagnose pancreatic cancer, as well as blood tests to measure tumor markers. Treatment for pancreatic cancer typically involves surgery, chemotherapy, and radiation therapy, although the prognosis is often poor due to the aggressive nature of the disease.
What are the symptoms of acute pancreatitis?
+The symptoms of acute pancreatitis can vary in severity, but common signs include severe abdominal pain, nausea, vomiting, and fever.
How is chronic pancreatitis diagnosed?
+Diagnosing chronic pancreatitis can be challenging, as the symptoms can be similar to those of other conditions. Imaging tests, such as CT scans and MRI, can help diagnose chronic pancreatitis, as well as blood tests to measure pancreatic enzyme levels.
What is the prognosis for pancreatic cancer?
+The prognosis for pancreatic cancer is often poor, with a 5-year survival rate of around 9% for patients diagnosed with pancreatic adenocarcinoma.
Meta Description: Learn about the different medical conditions that can affect the pancreas, including acute pancreatitis, chronic pancreatitis, diabetes mellitus, and pancreatic cancer. Understand the causes, symptoms, diagnosis, and treatment options for each condition.