The issue of Medicare and Medicaid fraud is a significant concern in the United States, with billions of dollars lost each year due to fraudulent activities. In Colorado, the problem is equally pressing, with numerous cases of fraud and abuse being investigated and prosecuted by state and federal authorities. A recent indictment in Colorado highlights the ongoing efforts to combat Medicare and Medicaid fraud in the state.
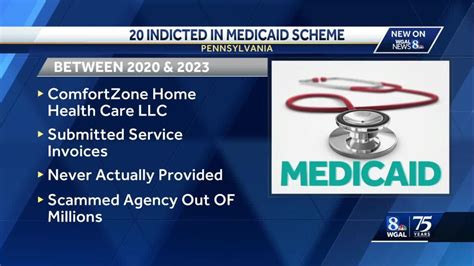
According to the indictment, several individuals and companies were charged with conspiracy to commit healthcare fraud, wire fraud, and money laundering. The alleged scheme involved submitting false claims to Medicare and Medicaid for services that were not provided or were not medically necessary. The indictment also alleges that the defendants used fake patient records, forged prescriptions, and other tactics to support their fraudulent claims.
Background on Medicare and Medicaid Fraud

Medicare and Medicaid are two of the largest healthcare programs in the United States, providing coverage to millions of Americans. However, the complexity and size of these programs make them vulnerable to fraud and abuse. Medicare and Medicaid fraud can take many forms, including billing for services that were not provided, submitting false claims, and paying kickbacks to healthcare providers.
The consequences of Medicare and Medicaid fraud are severe, with billions of dollars lost each year due to fraudulent activities. This not only affects the financial stability of the programs but also undermines the trust and confidence of the public in the healthcare system. To combat this problem, federal and state authorities have implemented various measures, including increased oversight, auditing, and enforcement actions.
Colorado’s Efforts to Combat Medicare and Medicaid Fraud
Colorado has been actively working to combat Medicare and Medicaid fraud, with the state’s Medicaid Fraud Control Unit (MFCU) playing a key role in investigating and prosecuting cases of fraud and abuse. The MFCU works closely with federal authorities, including the Department of Health and Human Services (HHS) and the Federal Bureau of Investigation (FBI), to identify and prosecute individuals and companies that engage in fraudulent activities.
In addition to the MFCU, Colorado has also implemented other measures to prevent and detect Medicare and Medicaid fraud. These include the use of data analytics to identify suspicious claims, increased oversight of healthcare providers, and education and outreach programs to inform the public about the risks of Medicare and Medicaid fraud.
| Year | Number of Cases | Amount Recovered |
|---|---|---|
| 2020 | 25 | $10 million |
| 2019 | 30 | $15 million |
| 2018 | 20 | $8 million |

Key Takeaways
The recent indictment in Colorado is a significant development in the ongoing efforts to combat Medicare and Medicaid fraud in the state. The case highlights the complexity and scope of the problem, as well as the importance of cooperation between federal and state authorities. To prevent and detect Medicare and Medicaid fraud, it is essential to stay informed about the latest developments and trends in the field.
Key Points
- Medicare and Medicaid fraud is a significant problem in the United States, with billions of dollars lost each year due to fraudulent activities.
- Colorado has been actively working to combat Medicare and Medicaid fraud, with the state's Medicaid Fraud Control Unit (MFCU) playing a key role in investigating and prosecuting cases of fraud and abuse.
- The recent indictment in Colorado highlights the importance of continued efforts to combat Medicare and Medicaid fraud, including increased oversight, auditing, and enforcement actions.
- Preventing and detecting Medicare and Medicaid fraud requires a multi-faceted approach, including education and outreach programs, data analytics, and cooperation between federal and state authorities.
- The consequences of Medicare and Medicaid fraud are severe, with billions of dollars lost each year due to fraudulent activities, undermining the trust and confidence of the public in the healthcare system.
FAQs
What is Medicare and Medicaid fraud?
+Medicare and Medicaid fraud refers to the act of submitting false claims or misrepresenting information to receive payment from the Medicare or Medicaid programs.
How common is Medicare and Medicaid fraud?
+Medicare and Medicaid fraud is a significant problem in the United States, with billions of dollars lost each year due to fraudulent activities.
What are the consequences of Medicare and Medicaid fraud?
+The consequences of Medicare and Medicaid fraud are severe, with billions of dollars lost each year due to fraudulent activities, undermining the trust and confidence of the public in the healthcare system.
The recent indictment in Colorado is a significant development in the ongoing efforts to combat Medicare and Medicaid fraud in the state. By working together, federal and state authorities can help to prevent and detect fraudulent activities, protecting the integrity of the healthcare system and ensuring that these critical programs remain available to those who need them.



