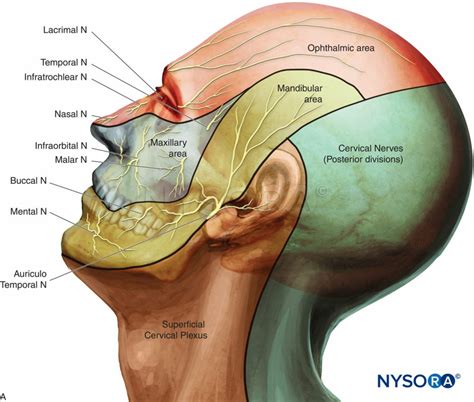
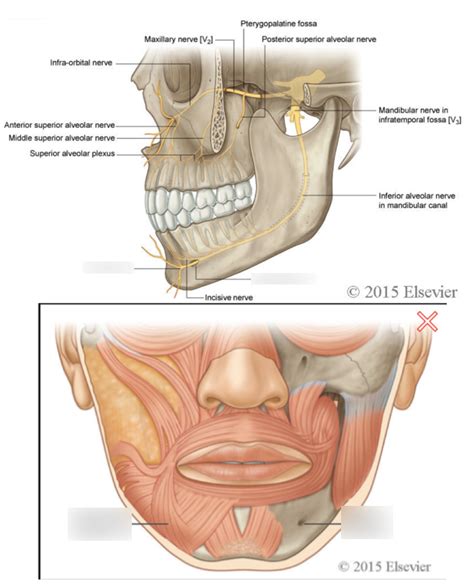
The mental nerve, also known as the mentalis nerve, is a branch of the inferior alveolar nerve, which itself is a branch of the mandibular division of the trigeminal nerve (cranial nerve V). This nerve plays a crucial role in providing sensory innervation to the lower lip, the mental region of the chin, and the surrounding gingiva. The mental nerve is significant in various dental and medical procedures, including local anesthesia, nerve repair, and diagnosing conditions such as nerve trauma or neuropathic pain.
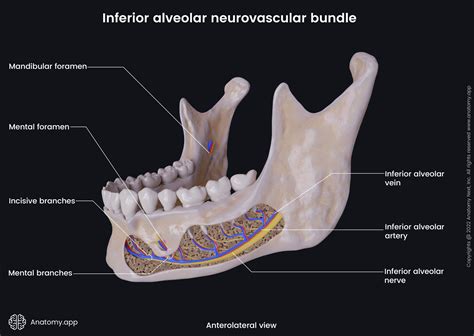
Understanding the anatomy and function of the mental nerve is essential for professionals in the dental and medical fields. The nerve originates from the inferior alveolar nerve, which runs within the mandibular canal of the lower jaw. Before exiting the mental foramen, located on either side of the chin, the mental nerve divides into two branches: the incisive and mental branches. The incisive branch continues within the incisive canal to innervate the lower anterior teeth and surrounding gingiva, while the mental branch exits the mental foramen to supply the skin of the chin and the lower lip.
Key Points
- The mental nerve is a branch of the inferior alveolar nerve, providing sensory innervation to the lower lip and chin.
- It exits the mandible through the mental foramen, located on either side of the chin, and divides into incisive and mental branches.
- The incisive branch innervates the lower anterior teeth and surrounding gingiva, while the mental branch supplies the skin of the chin and lower lip.
- Understanding the mental nerve's anatomy is crucial for dental and medical procedures, including local anesthesia and nerve repair.
- Damage to the mental nerve can result in numbness, pain, or altered sensation in the areas it innervates, necessitating proper diagnosis and treatment.
Anatomical Considerations and Clinical Significance
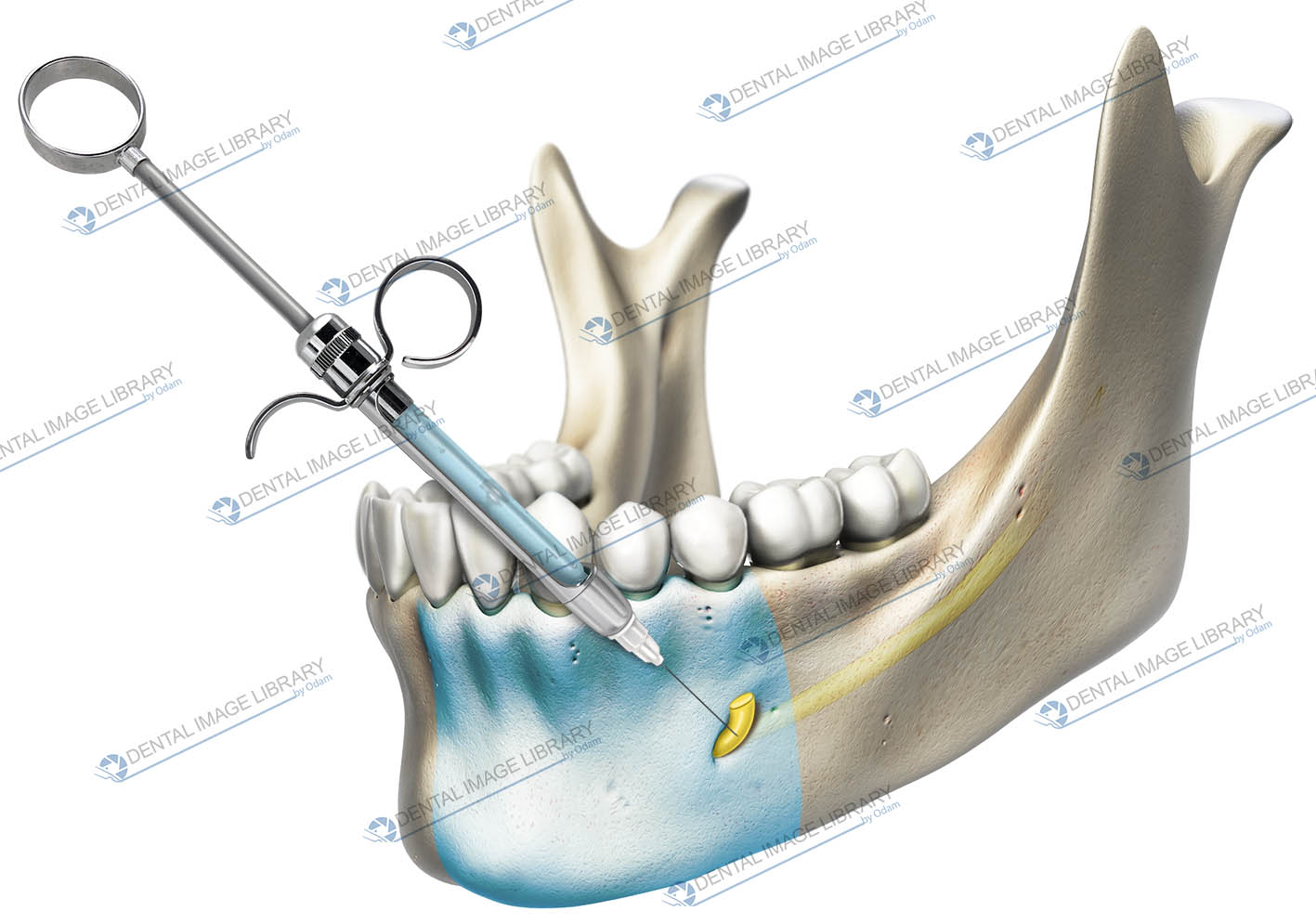
The mental nerve’s course and termination are of great importance in clinical practice. For instance, in dental procedures requiring local anesthesia, accurate knowledge of the nerve’s location is necessary to avoid needle trauma and ensure effective pain management. Similarly, during surgical procedures in the mental region, such as dental implant placement or orthognathic surgery, preserving the mental nerve is vital to prevent post-operative numbness or neuropathic pain.
Diagnosis and Management of Mental Nerve Injuries
Injuries to the mental nerve can occur due to various reasons, including dental procedures, facial trauma, or systemic conditions affecting the nerve. Diagnosis typically involves clinical examination, including sensory testing to assess the extent of nerve damage. Management strategies range from observation and conservative treatment for mild injuries to surgical intervention for more severe cases, aiming to relieve symptoms and restore nerve function.
| Condition | Clinical Presentation | Treatment |
|---|---|---|
| Mental Nerve Injury | Numbness, pain, or altered sensation in the lower lip and chin | Conservative management, surgical repair, or nerve repositioning |
| Neuropathic Pain | Chronic pain, burning, or tingling in the distribution of the mental nerve | Pharmacological management, nerve blocks, or surgical intervention |
| Trigeminal Neuralgia | Episodic, severe pain in the face, potentially involving the mental nerve distribution | Medical management with anticonvulsants or carbamazepine, surgical options for refractory cases |
Evolutionary and Historical Perspectives
Historically, understanding of the mental nerve and its role in facial sensation has evolved significantly. From early anatomical descriptions to modern clinical applications, the mental nerve has been a subject of interest due to its accessibility and the functional importance of the areas it innervates. Evolutionarily, the development of the trigeminal nerve, including its mandibular division from which the mental nerve originates, reflects the complex sensory and motor requirements of the face and jaws in vertebrates.
Modern Diagnostic and Therapeutic Approaches
Advances in diagnostic imaging, such as high-resolution MRI and CT scans, have improved the ability to visualize the mental nerve and its surrounding structures, aiding in the diagnosis of nerve injuries and other conditions. Therapeutically, developments in microsurgical techniques, nerve guides, and bioactive materials have expanded the possibilities for nerve repair and regeneration, offering new hope for patients with mental nerve injuries.
In conclusion, the mental nerve is a critical component of the sensory innervation of the lower face, with significant implications for dental and medical practice. Its unique anatomy, clinical significance, and the potential for injury highlight the need for careful consideration in procedural planning and execution. As our understanding of nerve biology and regenerative medicine continues to evolve, so too will the approaches to managing mental nerve injuries and related conditions, ultimately improving patient care and outcomes.
What is the primary function of the mental nerve?
+The primary function of the mental nerve is to provide sensory innervation to the lower lip, the mental region of the chin, and the surrounding gingiva.
Where does the mental nerve originate from?
+The mental nerve originates from the inferior alveolar nerve, which is a branch of the mandibular division of the trigeminal nerve (cranial nerve V).
What are the potential consequences of damaging the mental nerve?
+Damaging the mental nerve can result in numbness, pain, or altered sensation in the areas it innervates, which may necessitate proper diagnosis and treatment to alleviate symptoms and restore nerve function.