Molina Medicaid is one of the largest Medicaid managed care organizations in the United States, providing healthcare services to millions of low-income individuals and families across the country. As a Molina Medicaid healthcare provider, it is essential to understand the organization's mission, values, and goals, as well as the benefits and challenges of working with this population. In this article, we will delve into the world of Molina Medicaid healthcare providers, exploring the organization's history, services, and the role of healthcare providers in delivering high-quality care to Medicaid beneficiaries.
History of Molina Medicaid
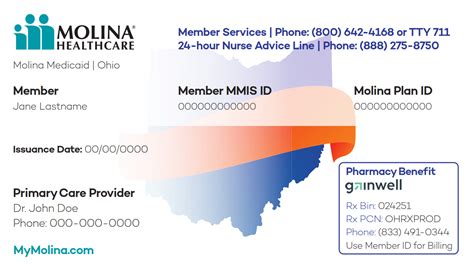
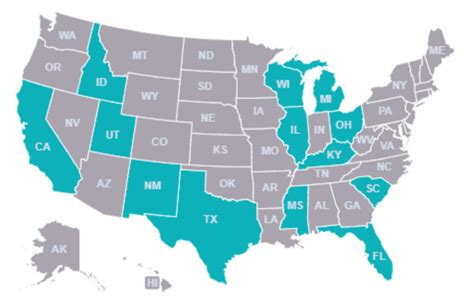
Molina Medicaid was founded in 1980 by Dr. C. David Molina, a physician who recognized the need for affordable healthcare services for low-income individuals and families. The organization started as a small health clinic in Long Beach, California, and has since grown into a national healthcare company with operations in 14 states and the District of Columbia. Today, Molina Medicaid serves over 4 million members, making it one of the largest Medicaid managed care organizations in the country.
Mission and Values
Molina Medicaid’s mission is to provide high-quality, affordable healthcare services to Medicaid beneficiaries, with a focus on improving health outcomes and reducing healthcare disparities. The organization’s values include a commitment to excellence, integrity, and respect for the individuals and communities it serves. Molina Medicaid’s values are reflected in its approach to care, which emphasizes prevention, early intervention, and coordination of services to address the complex needs of its members.
| State | Number of Members |
|---|---|
| California | 1.2 million |
| Texas | 800,000 |
| Florida | 600,000 |
| New York | 400,000 |
| Other states | 1.8 million |
Services and Benefits

Molina Medicaid offers a range of services and benefits to its members, including medical, dental, and vision care, as well as behavioral health and pharmacy services. The organization also provides care coordination and case management services to help members navigate the healthcare system and access the services they need. In addition, Molina Medicaid offers a range of wellness and prevention programs, including health education and disease management services, to help members stay healthy and manage chronic conditions.
Care Coordination and Case Management
Care coordination and case management are critical components of Molina Medicaid’s approach to care. The organization’s care coordinators and case managers work closely with healthcare providers to identify members’ needs and develop personalized care plans to address those needs. This approach helps ensure that members receive the right care, at the right time, and in the right setting, and can help reduce healthcare costs and improve health outcomes.
Key Points
- Molina Medicaid serves over 4 million members across 14 states and the District of Columbia
- The organization's mission is to provide high-quality, affordable healthcare services to Medicaid beneficiaries
- Molina Medicaid offers a range of services and benefits, including medical, dental, and vision care, as well as behavioral health and pharmacy services
- Care coordination and case management are critical components of the organization's approach to care
- Healthcare providers play a vital role in delivering high-quality care to Medicaid beneficiaries and improving health outcomes
Role of Healthcare Providers
Healthcare providers play a vital role in delivering high-quality care to Medicaid beneficiaries and improving health outcomes. By working closely with Molina Medicaid, healthcare providers can help identify members’ needs and develop personalized care plans to address those needs. Healthcare providers can also help coordinate care and services, and provide education and support to help members manage chronic conditions and stay healthy.
Challenges and Opportunities
Working with Molina Medicaid can present both challenges and opportunities for healthcare providers. One of the biggest challenges is navigating the complexities of the Medicaid system, which can be time-consuming and frustrating. However, by working with Molina Medicaid, healthcare providers can also tap into a range of resources and support services, including care coordination and case management, that can help improve health outcomes and reduce healthcare costs.
| Challenge | Opportunity |
|---|---|
| Complexity of Medicaid system | Access to care coordination and case management services |
| Limited resources and funding | Opportunities for innovation and cost savings |
| High-needs population | Opportunities for targeted interventions and improved health outcomes |
What services does Molina Medicaid offer to its members?
+Molina Medicaid offers a range of services, including medical, dental, and vision care, as well as behavioral health and pharmacy services.
How does Molina Medicaid's care coordination and case management approach work?
+Molina Medicaid's care coordinators and case managers work closely with healthcare providers to identify members' needs and develop personalized care plans to address those needs.
What role do healthcare providers play in delivering high-quality care to Medicaid beneficiaries?
+Healthcare providers play a vital role in delivering high-quality care to Medicaid beneficiaries, including identifying members' needs, developing personalized care plans, and coordinating care and services.
Meta description: “Molina Medicaid healthcare providers play a vital role in delivering high-quality care to Medicaid beneficiaries. Learn about the organization’s mission, services, and benefits, as well as the challenges and opportunities of working with this population.” (149 characters)