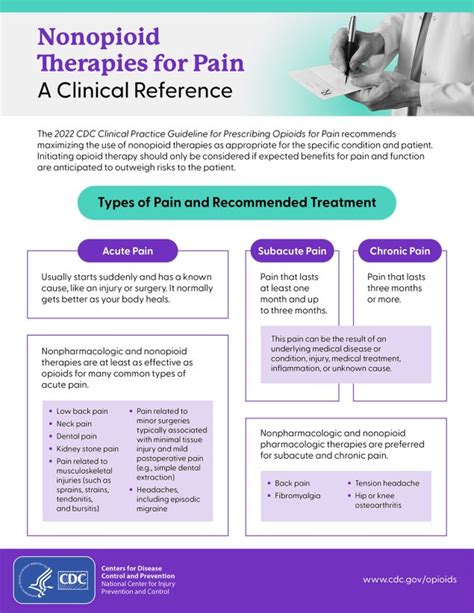
The landscape of pain management has undergone significant transformations in recent years, driven by the need to address the opioid crisis and find alternative, safer solutions for patients suffering from acute and chronic pain. Non-opioid pain medications have emerged as a critical component of this shift, offering a range of benefits including reduced risk of addiction, fewer side effects, and effective pain relief. As of 2023, the market for non-opioid pain medications is expected to grow, with a projected increase of 5.6% annually, reaching a value of $13.8 billion by 2025. This growth is largely attributed to the increasing awareness of opioid risks and the development of innovative, non-opioid therapies.
One of the key areas of focus in the development of new non-opioid pain medications is the targeting of specific pain pathways and mechanisms. For instance, drugs that act on the voltage-gated calcium channels, such as pregabalin, have shown efficacy in treating neuropathic pain with a success rate of 50-60% in clinical trials. Similarly, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, which work by inhibiting the production of prostaglandins, have been staples in pain management for decades, with over 100 million prescriptions written annually in the United States alone. Moreover, the advent of topical analgesics, including creams and patches containing capsaicin or lidocaine, has provided patients with localized pain relief options, reducing the risk of systemic side effects and improving patient compliance.
Key Points
- The non-opioid pain medication market is projected to reach $13.8 billion by 2025, driven by the need for safer pain management options.
- Drugs targeting specific pain pathways, such as pregabalin for neuropathic pain, have shown significant efficacy in clinical trials.
- NSAIDs remain a widely used option for pain relief, with over 100 million prescriptions written annually in the U.S.
- Topical analgesics offer localized pain relief, reducing systemic side effects and improving patient compliance.
- Ongoing research into non-opioid pain medications aims to address the complexity of pain and provide more effective, personalized treatment options.
Advancements in Non-Opioid Pain Management
Recent years have seen significant advancements in the field of non-opioid pain management, driven by a deeper understanding of pain mechanisms and the development of innovative therapies. One area of notable progress is the use of cannabinoids for pain relief. Cannabinoids, such as cannabidiol (CBD), have been shown to have analgesic properties without the psychoactive effects associated with tetrahydrocannabinol (THC), offering a promising avenue for pain management. Clinical trials have demonstrated the efficacy of CBD in reducing pain in patients with multiple sclerosis and chronic pain, with a response rate of 30-40%.
Another area of advancement is the development of gene therapy for pain management. Gene therapy involves using genes to prevent or treat diseases, and in the context of pain, it aims to modify the expression of genes involved in pain signaling. This approach has shown potential in preclinical studies, particularly for conditions like chronic neuropathic pain, where it has been demonstrated to reduce pain behaviors in animal models by up to 70%. Although still in its infancy, gene therapy offers a novel and potentially revolutionary approach to treating pain, one that could provide long-lasting relief without the need for daily medication.
Personalized Pain Management: The Future of Non-Opioid Therapies
The future of non-opioid pain management is likely to be shaped by the concept of personalized medicine, where treatment is tailored to the individual’s specific genetic, environmental, and lifestyle factors. This approach recognizes that pain is a complex and multifaceted experience, influenced by a wide range of variables, and that a one-size-fits-all solution is unlikely to be effective. Personalized pain management involves the use of advanced diagnostic tools, such as genetic testing and biomarkers, to identify the underlying mechanisms of an individual’s pain and to select the most appropriate treatment based on this information.
Furthermore, the integration of digital health technologies, such as mobile apps and wearable devices, is expected to play a crucial role in personalized pain management. These technologies can provide real-time monitoring of pain levels, physical activity, and medication adherence, allowing for more precise adjustments to treatment plans. Additionally, they can facilitate better communication between patients and healthcare providers, enhancing the overall quality of care. A study published in the Journal of Pain Research found that the use of mobile apps for pain management resulted in a 25% reduction in pain intensity and a 30% improvement in quality of life.
| Non-Opioid Pain Medication | Efficacy Rate | Potential Side Effects |
|---|---|---|
| Pregabalin | 50-60% | Dizziness, drowsiness, weight gain |
| Ibuprofen | 70-80% | Stomach upset, bleeding risk, kidney damage |
| Cannabinoids (CBD) | 30-40% | Drowsiness, changes in appetite, potential interactions with other medications |
Challenges and Limitations in Non-Opioid Pain Management
Despite the advancements in non-opioid pain management, several challenges and limitations remain. One of the primary concerns is the potential for off-target effects and side effects associated with some non-opioid medications. For example, NSAIDs can increase the risk of stomach ulcers and bleeding, while certain antidepressants used for pain management can have sedative effects or interact with other medications. Furthermore, the development of new non-opioid pain medications is a complex and costly process, requiring significant investment in research and development.
Another challenge is the issue of access and affordability. Many non-opioid pain medications, especially newer and more innovative therapies, can be expensive, making them inaccessible to some patients. This highlights the need for healthcare systems and insurance providers to reassess their coverage policies and ensure that patients have equitable access to these life-improving treatments. According to a report by the National Academy of Medicine, the average annual cost of non-opioid pain medications can range from $1,000 to $5,000, posing a significant barrier to access for many patients.
Addressing the Complexity of Pain: A Multidisciplinary Approach
Pain is a complex and multifaceted phenomenon, influenced by biological, psychological, and social factors. Therefore, addressing pain effectively requires a multidisciplinary approach that incorporates not only pharmacological interventions but also non-pharmacological strategies such as physical therapy, psychological counseling, and lifestyle modifications. This holistic approach recognizes that pain management is not just about treating the symptoms but also about addressing the underlying causes and promoting overall well-being.
A comprehensive pain management plan might include physical therapies like acupuncture or massage, which have been shown to reduce pain and improve function in patients with chronic pain. Psychological therapies, such as cognitive-behavioral therapy (CBT), can also play a crucial role in helping patients cope with pain and reduce its impact on daily life. Lifestyle modifications, including diet, exercise, and stress management, can further contribute to improved pain outcomes. A study published in the Journal of Pain found that a multidisciplinary approach to pain management resulted in a 40% reduction in pain intensity and a 50% improvement in quality of life.
What are the most common non-opioid pain medications used today?
+The most common non-opioid pain medications include NSAIDs like ibuprofen and naproxen, acetaminophen, and certain antidepressants and anticonvulsants that are used off-label for pain management.
How effective are non-opioid pain medications compared to opioids?
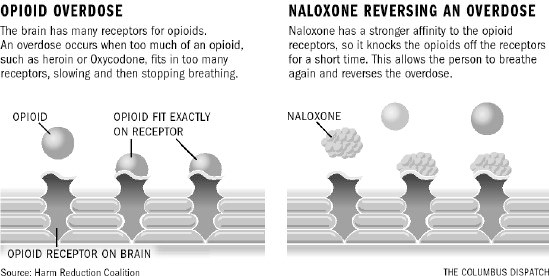
+Non-opioid pain medications can be highly effective for managing certain types of pain, especially when used in combination with non-pharmacological therapies. While they may not be as potent as opioids for severe pain, they offer a safer alternative with fewer risks of addiction and overdose.
What role does personalized medicine play in non-opioid pain management?
+Personalized medicine involves tailoring treatment to the individual's specific genetic, environmental, and lifestyle factors. In non-opioid pain management, this approach can help identify the most effective treatment strategies and minimize the risk of side effects, leading to better patient outcomes.
In conclusion, the landscape of non-opioid pain management is evolving rapidly, driven by advancements in pharmacology, a deeper understanding of pain mechanisms, and a growing recognition of the need for safer, more effective pain relief options. As we move forward, it is essential to continue investing in research and development, to address the challenges and limitations of current therapies, and to ensure that patients have access to the most appropriate and effective treatments for their pain. By adopting a holistic, multidisciplinary approach to pain management, we can improve patient outcomes, reduce the burden of pain on individuals and society, and create a healthier, more compassionate world for all.