The electrocardiogram (ECG) is a crucial diagnostic tool in cardiology, providing valuable insights into the heart's electrical activity. Among the various components of an ECG, the T wave is a significant aspect, as it reflects the repolarization of the ventricles. A non-specific T wave abnormality (NSTWA) is a common finding in ECG interpretations, often leaving clinicians with a dilemma in terms of diagnosis and management. In this article, we will delve into the nuances of non-specific T wave abnormalities, exploring their definitions, causes, clinical implications, and management strategies.
Definition and Classification
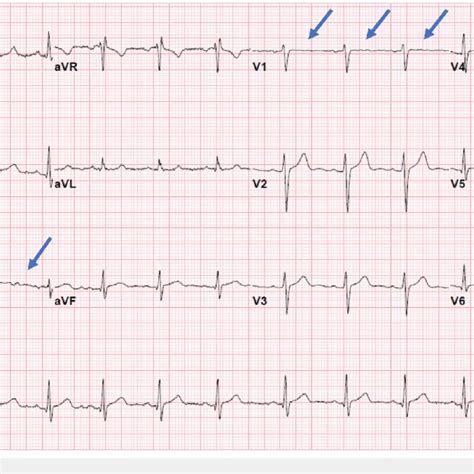
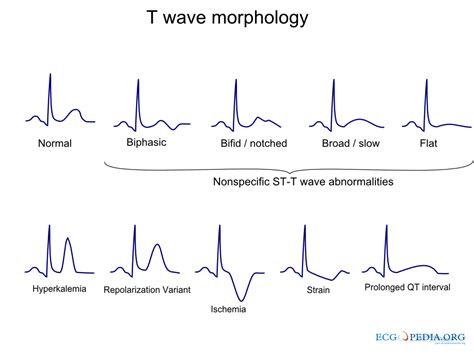
A non-specific T wave abnormality refers to any deviation in the T wave morphology that does not meet the specific criteria for other defined conditions, such as myocardial infarction, ventricular hypertrophy, or bundle branch blocks. These abnormalities can manifest as T wave flattening, inversion, or asymmetry, and may be localized to specific leads or diffuse across the ECG. The classification of T wave abnormalities is largely descriptive, with no universally accepted criteria for what constitutes a non-specific abnormality.
Clinical Context and Prevalence
NSTWAs are encountered in a significant proportion of ECGs, with studies suggesting that up to 10% of the general population may exhibit some form of T wave abnormality. The prevalence increases with age and in the presence of underlying cardiovascular conditions. However, the clinical significance of these abnormalities varies widely, ranging from benign variants to markers of underlying cardiac disease.
| Category | Prevalence |
|---|---|
| General Population | Up to 10% |
| Age > 60 years | Up to 20% |
| Cardiovascular Disease | Up to 30% |
Clinical Implications and Management
The management of patients with non-specific T wave abnormalities depends on the presence of symptoms and underlying cardiac conditions. Asymptomatic individuals with isolated T wave abnormalities may not require further evaluation, whereas those with symptoms suggestive of cardiac disease (e.g., chest pain, dyspnea) warrant a comprehensive assessment, including echocardiography, stress testing, and potentially, cardiac catheterization.
Differential Diagnosis
The differential diagnosis for non-specific T wave abnormalities is broad, encompassing various cardiac and non-cardiac conditions. These include myocardial ischemia, ventricular hypertrophy, cardiomyopathies, electrolyte imbalances, and drugs affecting repolarization. A thorough clinical evaluation, supplemented by targeted diagnostic testing, is crucial for establishing the underlying cause of the T wave abnormality.
Key Points
- NSTWAs are common ECG findings with variable clinical significance.
- Clinical context, including patient symptoms and medical history, is critical for interpretation.
- Asymptomatic individuals may not require further evaluation, whereas symptomatic patients warrant comprehensive assessment.
- Differential diagnosis is broad, necessitating a thorough clinical evaluation and targeted diagnostic testing.
- Management strategies depend on the underlying cause of the T wave abnormality.
Evidence-Based Practice and Future Directions
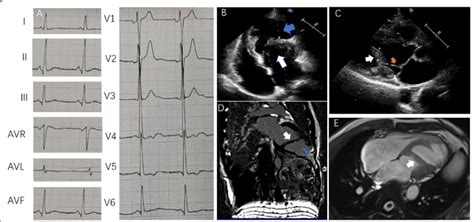
The approach to non-specific T wave abnormalities is evolving, with advances in ECG technology and our understanding of cardiac electrophysiology. High-resolution ECG and advanced signal processing techniques may enhance the detection and characterization of T wave abnormalities. Furthermore, the integration of ECG data with other diagnostic modalities, such as cardiac MRI, may improve the diagnostic accuracy and risk stratification of patients with NSTWAs.
Conclusion
In conclusion, non-specific T wave abnormalities are a common and complex entity in clinical cardiology. Their interpretation requires a deep understanding of ECG patterns, clinical context, and the nuances of cardiac disease. By adopting a nuanced and evidence-based approach, clinicians can optimize the management of patients with NSTWAs, ultimately improving outcomes and reducing unnecessary testing and interventions.
What is the clinical significance of non-specific T wave abnormalities?
+The clinical significance of non-specific T wave abnormalities varies widely, ranging from benign variants to markers of underlying cardiac disease. The presence of symptoms and underlying cardiac conditions influences the clinical approach and management.
How are non-specific T wave abnormalities managed?
+The management of patients with non-specific T wave abnormalities depends on the presence of symptoms and underlying cardiac conditions. Asymptomatic individuals may not require further evaluation, whereas those with symptoms suggestive of cardiac disease warrant a comprehensive assessment.
What is the role of advanced diagnostic testing in evaluating non-specific T wave abnormalities?
+Advanced diagnostic testing, such as echocardiography, stress testing, and cardiac catheterization, plays a crucial role in evaluating patients with non-specific T wave abnormalities, particularly those with symptoms suggestive of cardiac disease.