The role of Nurse Practitioners (NPs) in mental health care has become increasingly vital as the demand for mental health services continues to rise. With their advanced education and training, NPs are well-equipped to provide high-quality, patient-centered care to individuals with mental health conditions. In fact, according to the American Association of Nurse Practitioners (AANP), NPs are authorized to provide mental health services in all 50 states, and they are playing a crucial role in addressing the mental health workforce shortage. As of 2022, there are over 290,000 licensed NPs in the United States, with 7.3% of them specializing in psychiatric-mental health.
One of the key benefits of NPs in mental health care is their ability to provide comprehensive, holistic care that addresses the physical, emotional, and social needs of patients. This approach is particularly important in mental health, where patients often require coordinated care that involves multiple healthcare providers and community resources. NPs are trained to work collaboratively with other healthcare professionals, including psychiatrists, social workers, and psychologists, to ensure that patients receive seamless, evidence-based care. For example, a study published in the Journal of the American Psychiatric Nurses Association found that NPs who worked in collaborative care teams with psychiatrists and other healthcare professionals were able to improve patient outcomes and reduce symptoms of depression and anxiety.
Key Points
- NPs are authorized to provide mental health services in all 50 states and are playing a crucial role in addressing the mental health workforce shortage.
- NPs provide comprehensive, holistic care that addresses the physical, emotional, and social needs of patients with mental health conditions.
- NPs are trained to work collaboratively with other healthcare professionals to ensure that patients receive seamless, evidence-based care.
- NPs can prescribe medications, order diagnostic tests, and provide therapy and counseling services to patients with mental health conditions.
- NPs are particularly effective in providing mental health care in rural and underserved areas, where access to care is often limited.
The Role of NPs in Mental Health Care

NPs are qualified to provide a wide range of mental health services, including diagnosis, treatment, and management of mental health conditions. They can prescribe medications, order diagnostic tests, and provide therapy and counseling services to patients with mental health conditions such as depression, anxiety, bipolar disorder, and schizophrenia. In addition, NPs are trained to provide mental health services to patients across the lifespan, from children and adolescents to older adults. According to the Bureau of Labor Statistics, the employment of NPs is projected to grow 52% from 2020 to 2030, much faster than the average for all occupations.
Education and Training
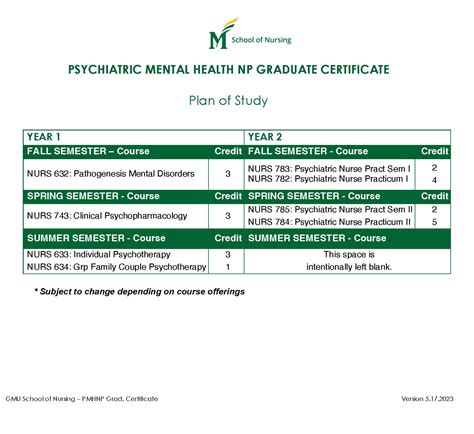
To become a psychiatric-mental health NP, one must complete a master’s or doctoral degree in nursing with a specialization in psychiatric-mental health. These programs typically include coursework in advanced pharmacology, pathophysiology, and health assessment, as well as clinical training in mental health settings. NPs must also obtain certification from the American Nurses Credentialing Center (ANCC) or the American Association of Nurse Practitioners (AANP) to practice as a psychiatric-mental health NP. The certification process involves passing a rigorous exam and completing continuing education requirements to stay current with the latest research and best practices in mental health care.
| Mental Health Condition | Prevalence | NP Services |
|---|---|---|
| Depression | 17.3% of adults in the United States (2020) | Medication management, therapy, counseling |
| Anxiety | 19.1% of adults in the United States (2020) | Medication management, therapy, counseling |
| Bipolar Disorder | 2.6% of adults in the United States (2020) | Medication management, therapy, counseling |
| Schizophrenia | 1.1% of adults in the United States (2020) | Medication management, therapy, counseling |
Challenges and Opportunities

Despite the many benefits of NPs in mental health care, there are several challenges and opportunities that must be addressed. One of the primary challenges is the shortage of mental health professionals, particularly in rural and underserved areas. NPs can help address this shortage by providing mental health services in these areas, where access to care is often limited. Another challenge is the lack of standardization in NP education and training programs, which can make it difficult for NPs to provide consistent, high-quality care. To address this challenge, professional organizations such as the AANP and the ANCC are working to develop standardized education and training programs for NPs.
There are also opportunities for NPs to play a larger role in mental health care, particularly in the areas of prevention and early intervention. By providing mental health services in primary care settings, NPs can help identify and treat mental health conditions early, reducing the risk of chronic disease and improving patient outcomes. Additionally, NPs can play a critical role in promoting mental health awareness and reducing stigma around mental illness, which is essential for improving mental health outcomes and reducing healthcare disparities.
What is the role of NPs in mental health care?
+NPs are qualified to provide a wide range of mental health services, including diagnosis, treatment, and management of mental health conditions. They can prescribe medications, order diagnostic tests, and provide therapy and counseling services to patients with mental health conditions.
How do NPs address the mental health workforce shortage?
+NPs can help address the mental health workforce shortage by providing mental health services in rural and underserved areas, where access to care is often limited. They can also provide mental health services in primary care settings, helping to identify and treat mental health conditions early and reduce the risk of chronic disease.
What are the challenges and opportunities for NPs in mental health care?
+Despite the many benefits of NPs in mental health care, there are several challenges and opportunities that must be addressed. These include the shortage of mental health professionals, particularly in rural and underserved areas, and the lack of standardization in NP education and training programs. Opportunities for NPs include providing mental health services in primary care settings, promoting mental health awareness, and reducing stigma around mental illness.
In conclusion, NPs play a vital role in mental health care, providing comprehensive, patient-centered care to individuals with mental health conditions. By addressing the mental health workforce shortage, promoting mental health awareness, and reducing stigma around mental illness, NPs can help improve patient outcomes, reduce healthcare costs, and enhance the overall quality of mental health services. As the demand for mental health services continues to rise, it’s essential that we recognize the critical role that NPs play in addressing this demand and provide them with the education, training, and resources they need to provide high-quality, evidence-based care.