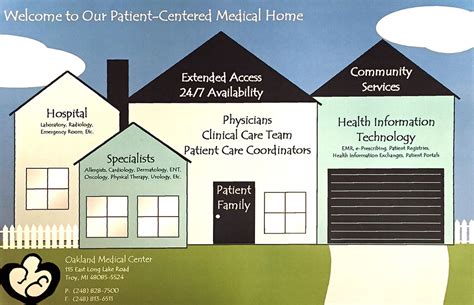
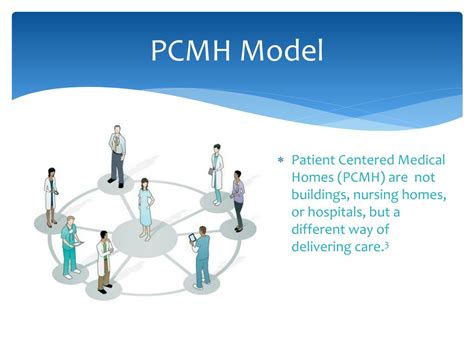
The Patient-Centered Medical Home (PCMH) is a healthcare delivery model that emphasizes patient-centered, comprehensive, and coordinated care. This approach has gained significant attention in recent years due to its potential to improve health outcomes, enhance patient satisfaction, and reduce healthcare costs. At its core, the PCMH model is designed to provide patients with a personalized and continuous relationship with a healthcare team, led by a primary care physician. The PCMH concept is built around five key principles: patient-centered care, comprehensive care, coordinated care, accessible care, and quality and safety.
One of the primary goals of the PCMH model is to provide patients with a medical home, where they can receive comprehensive and coordinated care. This approach is particularly important for patients with chronic conditions, such as diabetes or hypertension, who require ongoing management and monitoring. By providing patients with a medical home, healthcare providers can better manage chronic conditions, reduce hospitalizations, and improve health outcomes. According to a study published in the Journal of the American Medical Association (JAMA), patients who receive care in a PCMH setting are more likely to have their chronic conditions under control, compared to those who receive care in a traditional fee-for-service setting.
Key Components of the Patient-Centered Medical Home
The PCMH model is composed of several key components, including patient-centered care, comprehensive care, coordinated care, accessible care, and quality and safety. Patient-centered care is a critical component of the PCMH model, as it emphasizes the importance of patient preferences, values, and needs in the delivery of care. This approach requires healthcare providers to engage patients in decision-making, provide patients with access to their medical records, and involve patients in the development of their care plans. Comprehensive care is another key component of the PCMH model, as it requires healthcare providers to provide patients with a full range of services, including preventive care, acute care, and chronic care management.
Benefits of the Patient-Centered Medical Home
The PCMH model has been shown to have numerous benefits, including improved health outcomes, enhanced patient satisfaction, and reduced healthcare costs. According to a study published in the Annals of Family Medicine, patients who receive care in a PCMH setting are more likely to have improved health outcomes, compared to those who receive care in a traditional fee-for-service setting. The PCMH model has also been shown to reduce healthcare costs, by reducing hospitalizations and emergency department visits. A study published in the Journal of General Internal Medicine found that patients who receive care in a PCMH setting have lower healthcare costs, compared to those who receive care in a traditional fee-for-service setting.
| PCMH Component | Benefits |
|---|---|
| Patient-Centered Care | Improved patient satisfaction, enhanced patient engagement |
| Comprehensive Care | Improved health outcomes, reduced hospitalizations |
| Coordinated Care | Reduced healthcare costs, improved quality of care |
| Accessible Care | Increased patient access to care, reduced wait times |
| Quality and Safety | Improved patient safety, reduced medical errors |

Key Points
- The PCMH model is a healthcare delivery model that emphasizes patient-centered, comprehensive, and coordinated care.
- The PCMH model has been shown to improve health outcomes, enhance patient satisfaction, and reduce healthcare costs.
- Patient-centered care, comprehensive care, coordinated care, accessible care, and quality and safety are the five key principles of the PCMH model.
- The PCMH model has the potential to transform the way healthcare is delivered in the United States.
- Patients who receive care in a PCMH setting are more likely to have improved health outcomes, compared to those who receive care in a traditional fee-for-service setting.
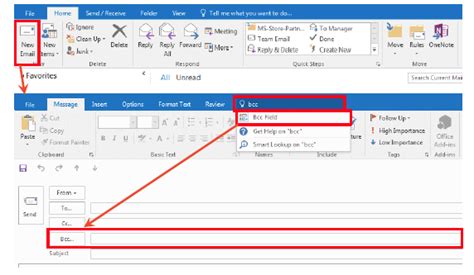
Despite the benefits of the PCMH model, there are several challenges to its implementation. One of the primary challenges is the need for significant changes in the way healthcare is delivered. The PCMH model requires healthcare providers to adopt a new approach to care, one that is patient-centered, comprehensive, and coordinated. This can be a significant challenge, particularly for healthcare providers who are used to a traditional fee-for-service model. Another challenge is the need for significant investments in technology and infrastructure. The PCMH model requires healthcare providers to have access to advanced technology, such as electronic health records and telehealth platforms, in order to provide patients with comprehensive and coordinated care.
According to a study published in the Journal of the American Medical Association (JAMA), the implementation of the PCMH model can be challenging, particularly for small and rural healthcare practices. The study found that these practices often lack the resources and infrastructure needed to implement the PCMH model, and may require significant support and guidance in order to make the transition. Despite these challenges, the PCMH model has the potential to transform the way healthcare is delivered in the United States, and to improve the health and well-being of patients.
Future Directions for the Patient-Centered Medical Home
The PCMH model is a dynamic and evolving concept, and there are several future directions for its development and implementation. One of the primary future directions is the integration of the PCMH model with other healthcare delivery models, such as the Accountable Care Organization (ACO) model. The ACO model is a healthcare delivery model that emphasizes accountability and coordination among healthcare providers, and has the potential to be integrated with the PCMH model to improve health outcomes and reduce healthcare costs. Another future direction is the use of advanced technology, such as artificial intelligence and machine learning, to support the delivery of care in a PCMH setting.
According to a report published by the National Committee for Quality Assurance (NCQA), the use of advanced technology has the potential to improve the delivery of care in a PCMH setting, by providing healthcare providers with access to real-time data and analytics. The report found that the use of advanced technology can help healthcare providers to identify high-risk patients, and to provide these patients with targeted interventions and support. The use of advanced technology can also help healthcare providers to improve the coordination of care, by providing patients with access to a comprehensive and integrated care plan.
What is the Patient-Centered Medical Home model?
+The Patient-Centered Medical Home (PCMH) model is a healthcare delivery model that emphasizes patient-centered, comprehensive, and coordinated care. It is designed to provide patients with a personalized and continuous relationship with a healthcare team, led by a primary care physician.
What are the benefits of the PCMH model?
+The PCMH model has been shown to improve health outcomes, enhance patient satisfaction, and reduce healthcare costs. It provides patients with a medical home, where they can receive comprehensive and coordinated care, and has the potential to transform the way healthcare is delivered in the United States.
What are the challenges to implementing the PCMH model?
+Despite the benefits of the PCMH model, there are several challenges to its implementation. One of the primary challenges is the need for significant changes in the way healthcare is delivered, and the need for significant investments in technology and infrastructure. Small and rural healthcare practices may also require significant support and guidance in order to make the transition to the PCMH model.
In conclusion, the Patient-Centered Medical Home model is a healthcare delivery model that emphasizes patient-centered, comprehensive, and coordinated care. It has the potential to improve health outcomes, enhance patient satisfaction, and reduce healthcare costs, and is a critical component of the future of healthcare in the United States. While there are challenges to its implementation, the PCMH model has the potential to transform the way healthcare is delivered, and to improve the health and well-being of patients.