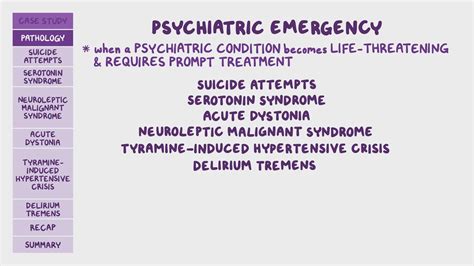
A psychiatric emergency is a situation where an individual's feelings, behaviors, or thoughts pose an immediate danger to themselves or others. It requires immediate intervention to prevent potential harm, and it is crucial to recognize the warning signs to provide timely and effective treatment. Psychiatric emergencies can arise from various conditions, including psychotic episodes, severe depression, anxiety disorders, and substance-induced psychosis, among others. The complex nature of these emergencies necessitates a comprehensive approach, incorporating both medical and psychological interventions.
The assessment of a psychiatric emergency involves a thorough evaluation of the individual's mental status, including their level of consciousness, orientation, thought processes, mood, and behavior. This assessment is critical in determining the severity of the situation and the appropriate course of action. Mental health professionals, such as psychiatrists and psychologists, play a pivotal role in this process, utilizing their expertise to diagnose and manage the underlying conditions contributing to the emergency. The involvement of family members or caregivers can also be invaluable, as they can provide essential information about the individual's history and current circumstances.
Key Points
- Psychiatric emergencies require immediate intervention to prevent harm to oneself or others.
- Conditions such as psychotic episodes, severe depression, and substance-induced psychosis can precipitate emergencies.
- A comprehensive assessment, including mental status evaluation, is crucial for determining the appropriate treatment.
- Mental health professionals are essential in the diagnosis and management of psychiatric emergencies.
- Family or caregiver involvement can provide critical information for effective intervention.
Causes and Risk Factors of Psychiatric Emergencies

Psychiatric emergencies can be precipitated by a variety of factors, including but not limited to, severe mental illness, substance abuse, and significant life stressors. Individuals with a history of psychiatric disorders are at a higher risk, as are those experiencing acute stress, such as the loss of a loved one, employment issues, or interpersonal conflicts. The interplay between genetic predisposition, environmental factors, and access to mental health services also plays a significant role in determining an individual’s risk of experiencing a psychiatric emergency.
Substance-Induced Psychosis
Substance-induced psychosis is a condition where the use of substances, such as drugs or alcohol, leads to psychotic symptoms. This can include hallucinations, delusions, and disorganized thinking and behavior. The risk of substance-induced psychosis is higher in individuals with a history of substance abuse and those using high doses of substances. Immediate medical attention is required to manage the symptoms and prevent further complications, such as withdrawal seizures or delirium tremens.
| Substance | Psychotic Symptoms |
|---|---|
| Cocaine | Paranoia, hallucinations |
| Methamphetamine | Delusions, disorganized thinking |
| Alcohol | Delirium tremens, hallucinations |
Management and Treatment of Psychiatric Emergencies

The management of psychiatric emergencies involves a multifaceted approach, incorporating both pharmacological and psychological interventions. Pharmacotherapy may include the use of antipsychotics, mood stabilizers, or antidepressants, depending on the underlying condition. Psychological interventions, such as crisis intervention, cognitive-behavioral therapy, and family therapy, can also be effective in managing the emergency and preventing future episodes.
Crisis Intervention
Crisis intervention is a short-term, intensive intervention aimed at stabilizing the individual and resolving the immediate crisis. It involves a thorough assessment of the situation, the development of a crisis plan, and the implementation of strategies to ensure the individual’s safety and the safety of others. Crisis intervention teams (CITs), which include mental health professionals, law enforcement officers, and emergency medical services personnel, play a critical role in managing psychiatric emergencies in the community.
The goal of crisis intervention is not only to manage the acute crisis but also to connect the individual with ongoing mental health services. This can include outpatient therapy, medication management, and support groups. The involvement of family members or caregivers in the crisis plan can also facilitate the individual's recovery and reintegration into their community.
What constitutes a psychiatric emergency?
+A psychiatric emergency is a situation where an individual's feelings, behaviors, or thoughts pose an immediate danger to themselves or others, requiring immediate intervention.
How are psychiatric emergencies managed?
+The management of psychiatric emergencies involves a comprehensive approach, including pharmacological interventions, psychological therapies, and crisis intervention, tailored to the individual's specific needs and circumstances.
What is the role of mental health professionals in psychiatric emergencies?
+Mental health professionals, such as psychiatrists and psychologists, play a pivotal role in the diagnosis, management, and treatment of psychiatric emergencies, utilizing their expertise to develop and implement effective treatment plans.
In conclusion, psychiatric emergencies are complex situations that require immediate attention and intervention to prevent harm to the individual or others. A comprehensive approach, incorporating both medical and psychological interventions, is essential for effective management and treatment. The expertise of mental health professionals, along with the support of family members or caregivers, is crucial in navigating these emergencies and ensuring the individual’s recovery and well-being.