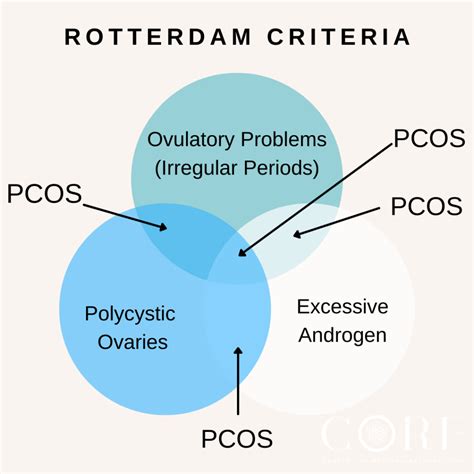
The Rotterdam Criteria for diagnosing Polycystic Ovary Syndrome (PCOS) were established in 2003 by the European Society for Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM). These criteria were developed to provide a more comprehensive and inclusive framework for diagnosing PCOS, as the previous criteria were considered too narrow. The Rotterdam Criteria require the presence of at least two of the following three features: oligo-ovulation or anovulation, clinical and/or biochemical signs of hyperandrogenism, and polycystic ovaries (PCO) on ultrasound, with the exclusion of other etiologies.
Background and Rationale
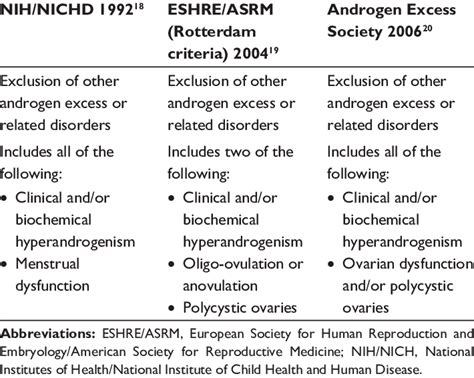
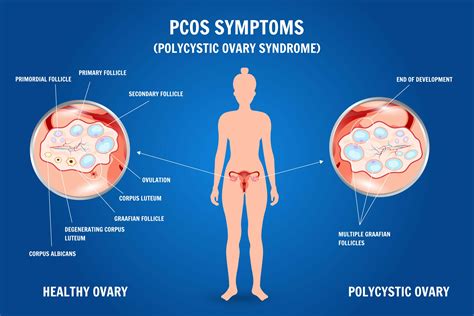
PCOS is a complex endocrine disorder that affects approximately 5-10% of women of reproductive age. It is characterized by a range of symptoms, including irregular menstrual cycles, hyperandrogenism, and polycystic ovaries. The Rotterdam Criteria were developed to address the limitations of the previous National Institutes of Health (NIH) criteria, which required the presence of all three features: oligo-ovulation, clinical or biochemical hyperandrogenism, and PCO on ultrasound. The NIH criteria were considered too restrictive, as many women with PCOS did not meet all three criteria.
Key Features of the Rotterdam Criteria
The Rotterdam Criteria are based on the presence of at least two of the following three features:
- Oligo-ovulation or anovulation: This refers to irregular menstrual cycles, with fewer than eight cycles per year, or no menstrual cycles at all.
- Clinical and/or biochemical signs of hyperandrogenism: This includes symptoms such as acne, hirsutism (excessive hair growth), and male-pattern baldness, as well as elevated levels of androgens (male hormones) in the blood.
- Polycystic ovaries (PCO) on ultrasound: This refers to the presence of 12 or more follicles in each ovary, with a diameter of 2-9 mm, and/or an ovarian volume of more than 10 mL.
The Rotterdam Criteria also require the exclusion of other etiologies that may mimic PCOS, such as congenital adrenal hyperplasia, androgen-secreting tumors, and Cushing's syndrome.
| Feature | Description |
|---|---|
| Oligo-ovulation or anovulation | Irregular menstrual cycles, with fewer than eight cycles per year, or no menstrual cycles at all |
| Clinical and/or biochemical signs of hyperandrogenism | Symptoms such as acne, hirsutism, and male-pattern baldness, as well as elevated levels of androgens in the blood |
| Polycystic ovaries (PCO) on ultrasound | Presence of 12 or more follicles in each ovary, with a diameter of 2-9 mm, and/or an ovarian volume of more than 10 mL |
Key Points
- The Rotterdam Criteria require the presence of at least two of the three features: oligo-ovulation or anovulation, clinical and/or biochemical signs of hyperandrogenism, and polycystic ovaries (PCO) on ultrasound
- The criteria exclude other etiologies that may mimic PCOS, such as congenital adrenal hyperplasia and androgen-secreting tumors
- The Rotterdam Criteria provide a more comprehensive framework for diagnosing PCOS, but are not universally accepted
- PCOS is a complex endocrine disorder that affects approximately 5-10% of women of reproductive age
- The diagnosis of PCOS should be based on a combination of clinical, biochemical, and ultrasound findings
Implications and Future Directions
The Rotterdam Criteria have significant implications for the diagnosis and management of PCOS. By providing a more comprehensive framework for diagnosis, the criteria can help identify women with PCOS who may not have met the previous NIH criteria. This can lead to earlier intervention and treatment, which can improve outcomes and reduce the risk of long-term complications, such as metabolic syndrome and cardiovascular disease.
Challenges and Limitations
Despite the advantages of the Rotterdam Criteria, there are still challenges and limitations to their use. One of the main limitations is the lack of universal acceptance, as some clinicians may still use the NIH criteria or other diagnostic frameworks. Additionally, the criteria may not be applicable to all populations, such as adolescents and women from different ethnic backgrounds.
What are the Rotterdam Criteria for PCOS?
+The Rotterdam Criteria are a set of diagnostic criteria for PCOS that require the presence of at least two of the three features: oligo-ovulation or anovulation, clinical and/or biochemical signs of hyperandrogenism, and polycystic ovaries (PCO) on ultrasound, with the exclusion of other etiologies.
How do the Rotterdam Criteria differ from the NIH criteria?
+The Rotterdam Criteria are more comprehensive and inclusive than the NIH criteria, as they require the presence of only two of the three features, rather than all three. This allows for the diagnosis of PCOS in women who may not have met the previous NIH criteria.
What are the implications of the Rotterdam Criteria for the diagnosis and management of PCOS?
+The Rotterdam Criteria have significant implications for the diagnosis and management of PCOS, as they can help identify women with PCOS who may not have met the previous NIH criteria. This can lead to earlier intervention and treatment, which can improve outcomes and reduce the risk of long-term complications.