Stress-induced fits, also known as stress-induced seizures or psychogenic non-epileptic seizures (PNES), are a complex and multifaceted phenomenon that has garnered significant attention in the medical and psychological communities. These events are characterized by sudden, temporary disruptions in behavior, consciousness, or motor control, often precipitated by intense emotional or psychological distress. It is essential to approach this topic with a nuanced understanding, recognizing the intricate interplay between psychological, neurological, and physiological factors that contribute to stress-induced fits.
The prevalence of stress-induced fits is not well-established, with estimates suggesting that they may account for up to 20% of patients presenting with seizure-like symptoms. However, it is crucial to note that these events are not necessarily equivalent to epileptic seizures, which are typically associated with abnormal electrical activity in the brain. Instead, stress-induced fits are often linked to underlying psychological or psychiatric conditions, such as anxiety, depression, or post-traumatic stress disorder (PTSD). A comprehensive understanding of these underlying factors is critical for developing effective treatment strategies and improving patient outcomes.
Key Points
- Stress-induced fits are a complex phenomenon with psychological, neurological, and physiological components
- These events are often precipitated by intense emotional or psychological distress
- Prevalence estimates suggest that stress-induced fits may account for up to 20% of patients presenting with seizure-like symptoms
- Underlying psychological or psychiatric conditions, such as anxiety or PTSD, are common comorbidities
- A comprehensive treatment approach, incorporating psychological, medical, and social interventions, is essential for improving patient outcomes
Pathophysiology and Mechanisms
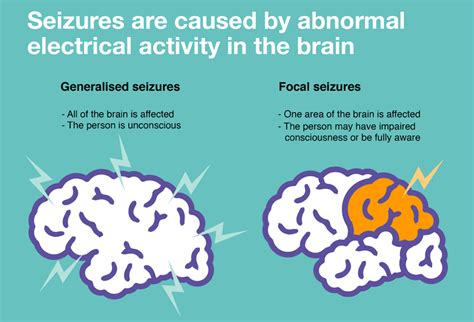
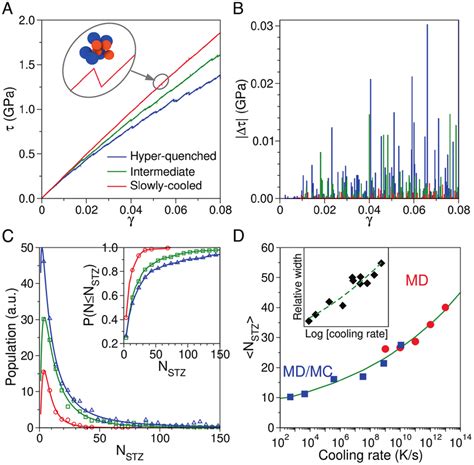
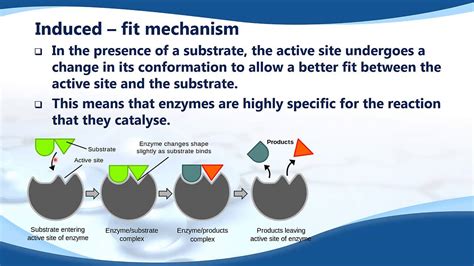
The pathophysiology of stress-induced fits is not fully understood, but research suggests that a complex interplay between psychological, neurological, and physiological factors contributes to these events. One key mechanism involves the activation of the body’s stress response system, which can lead to alterations in brain activity, particularly in regions involved in emotional processing and regulation. Additionally, changes in neurotransmitter levels, such as serotonin and dopamine, may also play a role in the development of stress-induced fits.
A study published in the journal Neurology found that patients with stress-induced fits exhibited altered functional connectivity between brain regions, including the amygdala, hippocampus, and prefrontal cortex. These findings suggest that stress-induced fits may be associated with disruptions in normal brain function, particularly in networks involved in emotional processing and regulation. Further research is needed to fully elucidate the underlying mechanisms and to develop effective treatment strategies.
Diagnosis and Assessment
Diagnosing stress-induced fits can be challenging, as these events often present with symptoms similar to those of epileptic seizures. A comprehensive diagnostic evaluation, incorporating clinical interviews, psychological assessments, and neurological examinations, is essential for distinguishing stress-induced fits from other conditions. The use of standardized assessment tools, such as the Minnesota Multiphasic Personality Inventory (MMPI) or the Beck Depression Inventory (BDI), can help identify underlying psychological or psychiatric conditions that may be contributing to these events.
| Diagnostic Criteria | Characteristics |
|---|---|
| 1. Presence of seizure-like symptoms | Transient, often dramatic, changes in behavior or consciousness |
| 2. Absence of abnormal electrical activity | No evidence of epileptiform discharges on electroencephalography (EEG) |
| 3. Presence of psychological or psychiatric comorbidity | Underlying conditions, such as anxiety, depression, or PTSD, that may be contributing to stress-induced fits |
Treatment and Management
Treatment of stress-induced fits typically involves a multidisciplinary approach, incorporating psychological, medical, and social interventions. Psychotherapy, such as cognitive-behavioral therapy (CBT) or dialectical behavior therapy (DBT), can help patients develop coping strategies and address underlying psychological or psychiatric conditions. Medications, such as antidepressants or anti-anxiety agents, may also be prescribed to help manage symptoms and reduce the frequency of stress-induced fits.
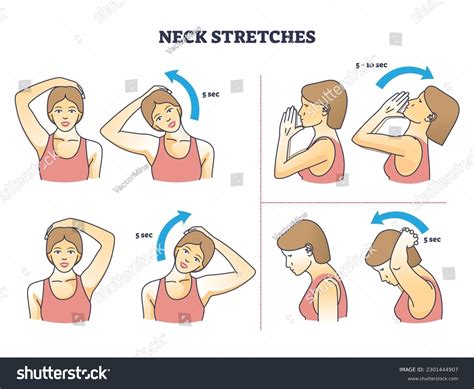
In addition to these interventions, lifestyle modifications, such as stress management techniques, relaxation training, and exercise, can help reduce the overall burden of stress and anxiety. A study published in the Journal of Clinical Psychology found that patients who received a combination of CBT and stress management training exhibited significant reductions in stress-induced fit frequency and severity. These findings highlight the importance of a comprehensive treatment approach, incorporating multiple interventions, to improve patient outcomes.
Future Directions
Further research is needed to fully understand the pathophysiology and mechanisms underlying stress-induced fits. The development of more effective treatment strategies, incorporating novel therapeutic approaches and technologies, is also critical for improving patient outcomes. The use of neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), may help elucidate the neural mechanisms involved in stress-induced fits and inform the development of more targeted interventions.
What are the most common triggers for stress-induced fits?
+Common triggers for stress-induced fits include intense emotional or psychological distress, such as anxiety, depression, or PTSD. Other triggers may include sleep deprivation, certain medications, or underlying medical conditions.
How can stress-induced fits be distinguished from epileptic seizures?
+Stress-induced fits can be distinguished from epileptic seizures through a comprehensive diagnostic evaluation, incorporating clinical interviews, psychological assessments, and neurological examinations. The absence of abnormal electrical activity on EEG and the presence of psychological or psychiatric comorbidity can help support a diagnosis of stress-induced fits.
What is the most effective treatment approach for stress-induced fits?
+A comprehensive treatment approach, incorporating psychotherapy, medication, and lifestyle modifications, is typically the most effective strategy for managing stress-induced fits. A multidisciplinary team, including psychologists, psychiatrists, and neurologists, can help develop a personalized treatment plan to address underlying psychological or psychiatric conditions and reduce the frequency and severity of stress-induced fits.
In conclusion, stress-induced fits are a complex and multifaceted phenomenon that requires a comprehensive treatment approach, incorporating psychological, medical, and social interventions. By recognizing the importance of psychological and psychiatric comorbidities and addressing these underlying conditions, patients can reduce the frequency and severity of stress-induced fits and improve their overall quality of life. Further research is needed to fully understand the pathophysiology and mechanisms underlying stress-induced fits and to develop more effective treatment strategies.