Alcohol consumption has been a longstanding aspect of human culture and social interactions, but its effects on health have been a subject of extensive study. Among the many health risks associated with alcohol consumption, the link between alcohol and cancer has been particularly well-documented. The relationship between alcohol intake and cancer risk is complex, involving various types of cancer and influenced by multiple factors including the amount and frequency of alcohol consumption, the type of alcoholic beverage, and individual susceptibility. This article aims to explore the five significant alcohol cancer risks, providing insights into the mechanisms by which alcohol increases cancer risk, the types of cancer most affected, and the implications for public health and individual behavior.
Key Points
- Alcohol consumption is associated with an increased risk of several types of cancer, including liver, breast, colon, esophageal, and head and neck cancers.
- The risk of cancer from alcohol consumption is dose-dependent, with higher intake leading to greater risk.
- Individual susceptibility, including genetic predisposition and other health conditions, can modify the risk of alcohol-related cancers.
- Public health strategies aimed at reducing alcohol consumption can contribute to lowering the incidence of alcohol-related cancers.
- Understanding the mechanisms by which alcohol increases cancer risk can inform prevention and intervention efforts.
Alcohol Metabolism and Cancer Risk

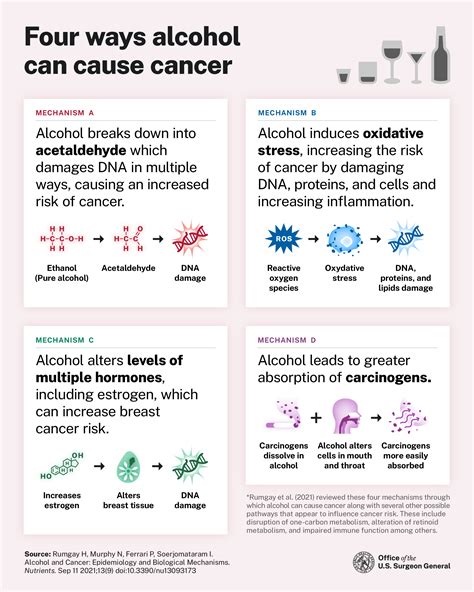
Alcohol is metabolized in the body primarily by the liver, where it is converted into acetaldehyde, a known carcinogen. This process can lead to genetic damage and disrupt normal cellular function, increasing the risk of cancer. Additionally, alcohol metabolism generates reactive oxygen species (ROS), which can cause oxidative stress and further contribute to carcinogenesis. The impact of alcohol on cancer risk is not limited to the liver; its metabolites and the oxidative stress it induces can affect various tissues and organs, contributing to the development of different types of cancer.
Liver Cancer
Liver cancer, particularly hepatocellular carcinoma (HCC), is strongly associated with alcohol consumption. Chronic alcohol intake can lead to liver cirrhosis, a condition characterized by scarring of the liver tissue, which significantly increases the risk of developing HCC. The risk is dose-dependent, with higher levels of alcohol consumption leading to a greater risk of liver cirrhosis and, subsequently, liver cancer. For example, a study found that consuming more than 50 grams of alcohol per day increases the risk of liver cancer by 3.3 times compared to non-drinkers.
| Type of Cancer | Relative Risk | Alcohol Consumption Level |
|---|---|---|
| Liver Cancer | 3.3 | >50 grams/day |
| Breast Cancer | 1.2 | 15-30 grams/day |
| Colon Cancer | 1.1 | 25-50 grams/day |
| Esophageal Cancer | 5.4 | >50 grams/day |
| Head and Neck Cancer | 2.6 | >50 grams/day |
Public Health Implications

The association between alcohol consumption and cancer risk has significant implications for public health. Strategies aimed at reducing alcohol intake, such as taxation on alcohol products, education campaigns, and restrictions on alcohol sales, can contribute to lowering the incidence of alcohol-related cancers. Additionally, early detection and screening programs can improve outcomes for individuals diagnosed with cancer. For instance, cost-effectiveness analyses of breast cancer screening have shown that these programs can be cost-effective in preventing breast cancer deaths.
Individual Susceptibility and Genetic Factors
Individual susceptibility, including genetic predisposition, plays a crucial role in the risk of developing alcohol-related cancers. Genetic variations can affect how alcohol is metabolized and how the body responds to alcohol-induced damage. For example, individuals with certain polymorphisms in the alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) genes may have a higher risk of alcohol-related cancers due to differences in alcohol metabolism. Understanding these genetic factors can help in identifying high-risk individuals and tailoring preventive measures accordingly.
Conclusion and Future Directions
In conclusion, the relationship between alcohol consumption and cancer risk is well-established, with significant implications for public health and individual behavior. Reducing alcohol intake is a critical step in lowering the risk of alcohol-related cancers. Future research should continue to explore the mechanisms by which alcohol increases cancer risk, the role of individual susceptibility, and the effectiveness of public health interventions aimed at reducing alcohol consumption. By advancing our understanding of these factors, we can develop more effective strategies for the prevention and control of alcohol-related cancers.
What is the primary mechanism by which alcohol increases cancer risk?
+The primary mechanism involves the metabolism of alcohol into acetaldehyde, a known carcinogen, and the generation of reactive oxygen species, leading to genetic damage and oxidative stress.
Which type of cancer is most strongly associated with alcohol consumption?
+Liver cancer, particularly hepatocellular carcinoma, is most strongly associated with alcohol consumption, with chronic alcohol intake leading to liver cirrhosis and significantly increasing the risk of developing liver cancer.
Can reducing alcohol intake lower the risk of alcohol-related cancers?
+Yes, reducing alcohol intake can lower the risk of alcohol-related cancers. Public health strategies aimed at reducing alcohol consumption, along with individual efforts to moderate drinking habits, are critical in the prevention of these cancers.



