The reporting of adverse events to regulatory authorities is a critical component of pharmacovigilance, playing a pivotal role in ensuring the safety of drugs and medical devices. Regulatory authorities worldwide, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), have established rigorous frameworks for the reporting of adverse events. These frameworks are designed to facilitate the timely detection of potential safety issues, thereby enabling prompt regulatory action to protect public health.
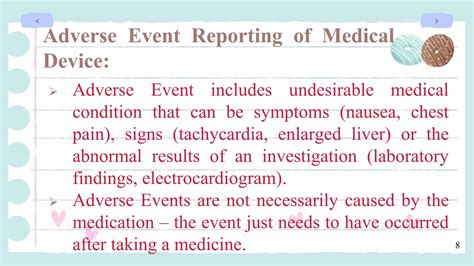
Adverse events, which can range from mild side effects to life-threatening conditions, are undesirable experiences associated with the use of a drug or medical device. The spontaneous reporting of adverse events by healthcare professionals and patients is a cornerstone of pharmacovigilance. This voluntary reporting, although subject to underreporting, provides valuable insights into the safety profile of marketed products. Regulatory authorities also mandate the reporting of adverse events during clinical trials and post-marketing surveillance, ensuring a comprehensive assessment of safety data throughout a product's lifecycle.
Key Points
- The timely reporting of adverse events to regulatory authorities is crucial for ensuring drug and medical device safety.
- Regulatory frameworks require the reporting of adverse events during clinical trials and post-marketing surveillance.
- Spontaneous reporting by healthcare professionals and patients, although voluntary, is a vital component of pharmacovigilance.
- Underreporting of adverse events can hinder the detection of safety issues, emphasizing the need for enhanced reporting practices.
- Regulatory authorities analyze reported adverse events to inform regulatory decisions and ensure public health protection.
Regulatory Frameworks for Adverse Event Reporting
Regulatory authorities have developed detailed guidelines and regulations for the reporting of adverse events. For instance, the FDA requires sponsors of clinical trials to report serious adverse events (SAEs) and unexpected adverse events to the agency within specific timeframes. Similarly, the EMA mandates the reporting of suspected adverse reactions, including those that are serious, unexpected, and related to the medicinal product. These regulatory frameworks ensure that adverse event data are systematically collected, evaluated, and acted upon to mitigate potential risks.
Types of Adverse Event Reports
Adverse event reports can be categorized into several types, including spontaneous reports, clinical trial reports, and periodic safety update reports (PSURs). Spontaneous reports are submitted voluntarily by healthcare professionals and patients, while clinical trial reports are generated during the conduct of clinical trials. PSURs are periodic reports that summarize the safety data of a medicinal product, providing an ongoing assessment of its risk-benefit profile. Each type of report contributes valuable information to the overall safety evaluation of drugs and medical devices.
| Report Type | Description |
|---|---|
| Spontaneous Reports | Voluntary reports submitted by healthcare professionals and patients. |
| Clinical Trial Reports | Reports generated during clinical trials to document adverse events. |
| Periodic Safety Update Reports (PSURs) | Periodic reports summarizing safety data to assess the risk-benefit profile of a medicinal product. |
Challenges in Adverse Event Reporting
Despite the importance of adverse event reporting, several challenges hinder its effectiveness. Underreporting is a significant issue, as not all adverse events are reported to regulatory authorities. This can be due to various factors, including lack of awareness, time constraints, and uncertainty about what constitutes a reportable event. Additionally, the quality of reported data can vary, with incomplete or inaccurate information potentially leading to misunderstandings or delays in regulatory action. To address these challenges, regulatory authorities and healthcare organizations are implementing strategies to enhance reporting practices, including education and training programs for healthcare professionals and the development of user-friendly reporting tools.
Improving Adverse Event Reporting
To optimize adverse event reporting, it is essential to foster a culture of transparency and safety within the healthcare community. This can be achieved through targeted education and training initiatives, which aim to increase awareness of the importance of reporting and provide guidance on the reporting process. Furthermore, leveraging technology, such as electronic reporting systems, can streamline the reporting process, reduce errors, and facilitate the timely submission of reports. Regulatory authorities also play a critical role in promoting adherence to reporting requirements through audits, inspections, and enforcement actions when necessary.
What constitutes an adverse event that should be reported to regulatory authorities?
+An adverse event is any undesirable experience associated with the use of a drug or medical device, including side effects, allergic reactions, and any other untoward medical occurrences. The reporting of adverse events is critical for ensuring the safety of these products.
Why is underreporting of adverse events a significant challenge in pharmacovigilance?
+Underreporting can lead to an incomplete understanding of the safety profile of drugs and medical devices, potentially resulting in delayed detection of safety issues and compromised public health protection. Factors contributing to underreporting include lack of awareness, time constraints, and uncertainty about reportable events.
How can the quality of adverse event reports be improved?
+The quality of adverse event reports can be enhanced through education and training programs for healthcare professionals, the use of standardized reporting forms, and the implementation of electronic reporting systems that facilitate accurate and timely data submission.
In conclusion, the reporting of adverse events to regulatory authorities is a vital process that underpins the safety of drugs and medical devices. While challenges such as underreporting and variable data quality exist, concerted efforts by regulatory authorities, healthcare organizations, and individuals can enhance reporting practices. By fostering a culture of safety, leveraging technology, and promoting adherence to reporting requirements, it is possible to optimize adverse event reporting and ensure the protection of public health.