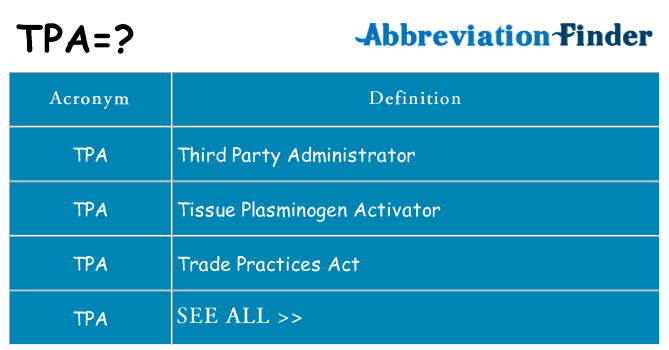
The medical abbreviation "TPA" has multiple meanings depending on the context in which it is used. In the field of medicine, TPA is often an abbreviation for "Tissue Plasminogen Activator." This refers to a protein that is involved in the breakdown of blood clots. Tissue Plasminogen Activator is used as a medication to treat conditions such as acute ischemic stroke, pulmonary embolism, and myocardial infarction (heart attack), by dissolving the blood clots that cause these conditions.
Tissue Plasminogen Activator (tPA) in Stroke Treatment
tPA is most notably used in the treatment of acute ischemic strokes. When administered promptly, ideally within 3 to 4.5 hours of the onset of stroke symptoms, tPA can significantly improve outcomes by restoring blood flow to the affected area of the brain, thereby limiting the extent of brain damage. The timing of tPA administration is critical, as the benefits of treatment decrease and the risks of complications, such as bleeding, increase with time.
Administration and Mechanism of Action
The administration of tPA involves intravenous infusion. Its mechanism of action involves converting plasminogen into plasmin, which then breaks down fibrin clots. This process is highly specific to the clot itself, minimizing the risk of systemic bleeding, although such risks cannot be entirely eliminated. The effectiveness and safety of tPA have been demonstrated in numerous clinical trials, leading to its widespread adoption as a standard treatment for eligible patients with acute ischemic stroke.
| Condition | Time Window for tPA Administration |
|---|---|
| Acute Ischemic Stroke | Within 3 to 4.5 hours of symptom onset |
| Pulmonary Embolism | Varies, often considered in massive or submassive cases |
| Myocardial Infarction (Heart Attack) | Varies, often considered in specific scenarios |
Key Points
- tPA stands for Tissue Plasminogen Activator, a medication used to dissolve blood clots.
- It is primarily used in the treatment of acute ischemic stroke, pulmonary embolism, and myocardial infarction.
- The timing of tPA administration is crucial, especially in stroke treatment, where it should be given within 3 to 4.5 hours of symptom onset.
- tPA works by converting plasminogen into plasmin, which breaks down fibrin clots.
- While effective, tPA carries risks, including bleeding, and its use must be carefully considered on a patient-by-patient basis.
Given the critical nature of tPA in emergency medicine, healthcare providers must be well-versed in its indications, administration, and potential complications. Continuous education and updates on the latest clinical guidelines are essential for maximizing the benefits of tPA while minimizing its risks.
What are the primary uses of TPA in medicine?
+TPA, or Tissue Plasminogen Activator, is primarily used to treat acute ischemic stroke, pulmonary embolism, and myocardial infarction by dissolving the blood clots that cause these conditions.
How does tPA work in the body?
+tPA works by converting plasminogen into plasmin, an enzyme that breaks down blood clots. This process helps restore blood flow to the affected area, reducing the risk of permanent damage.
What are the risks associated with tPA administration?
+The primary risk associated with tPA administration is bleeding. While tPA is designed to target clots specifically, there is a risk of systemic bleeding, including potentially life-threatening hemorrhages. The decision to administer tPA must be made carefully, weighing the potential benefits against these risks.
In conclusion, TPA plays a vital role in the management of acute vascular events, offering a potent tool for clinicians to improve patient outcomes. Its use, however, requires careful consideration of the benefits and risks, as well as adherence to established clinical guidelines to ensure safe and effective administration.