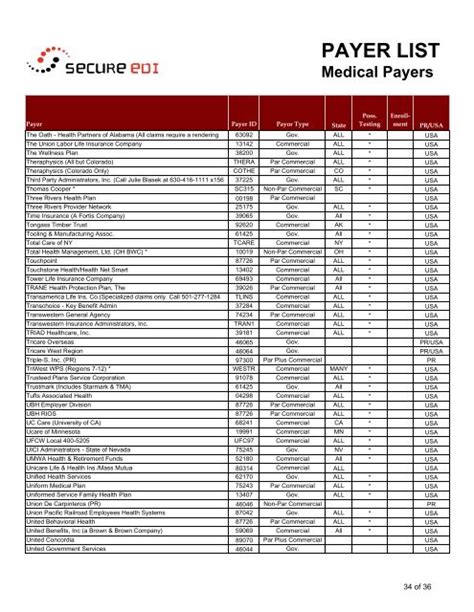
The U6885 Payer ID is a unique identifier used in the healthcare industry to facilitate electronic claims submission and payment processing. This identifier is crucial for healthcare providers and billing entities to ensure seamless communication with payers, such as insurance companies and government programs. The U6885 Payer ID is part of the standard protocol for electronic data interchange (EDI) in healthcare, which is governed by regulations like the Health Insurance Portability and Accountability Act (HIPAA) and managed by entities such as the Centers for Medicare and Medicaid Services (CMS) and the National Council for Prescription Drug Programs (NCPDP).
Understanding the Role of U6885 Payer ID
The U6885 Payer ID plays a significant role in the electronic claims processing system. It is used to identify the payer to whom the claim is being submitted. This identifier is essential for ensuring that claims are directed to the correct payer, facilitating timely and accurate payment processing. The use of a standardized identifier like the U6885 Payer ID helps reduce errors in claims submission and payment, streamlining the revenue cycle for healthcare providers. Moreover, it aids in the electronic remittance advice (ERA) process, where payers send explanations of benefits (EOBs) or electronic funds transfer (EFT) information to providers, further automating the payment process.
Implementation and Management
The implementation and management of the U6885 Payer ID involve several stakeholders, including healthcare providers, billing companies, payers, and clearinghouses. Clearinghouses act as intermediaries between providers and payers, facilitating the electronic transmission of claims and other healthcare transactions. They ensure that the U6885 Payer ID, along with other necessary information, is correctly formatted and submitted to the appropriate payer. The management of these identifiers requires ongoing updates and maintenance to reflect changes in payer information, ensuring that claims are processed efficiently and accurately.
| Payer Type | U6885 Payer ID Example | Description |
|---|---|---|
| Medicare | XXXXX | A unique identifier for Medicare claims |
| Medicaid | YYYYY | A unique identifier for Medicaid claims |
| Commercial Insurance | ZZZZZ | A unique identifier for commercial insurance claims |
Key Points
- The U6885 Payer ID is a unique identifier for payers in the healthcare industry, facilitating electronic claims submission and payment processing.
- It plays a crucial role in ensuring claims are directed to the correct payer, reducing errors and facilitating timely payment.
- Implementation and management involve stakeholders like healthcare providers, billing companies, payers, and clearinghouses.
- Ongoing updates and maintenance of the U6885 Payer ID are necessary to reflect changes in payer information.
- Regular verification and updating of the U6885 Payer IDs can prevent claim rejection and ensure timely payment.
Technical Specifications and Compliance
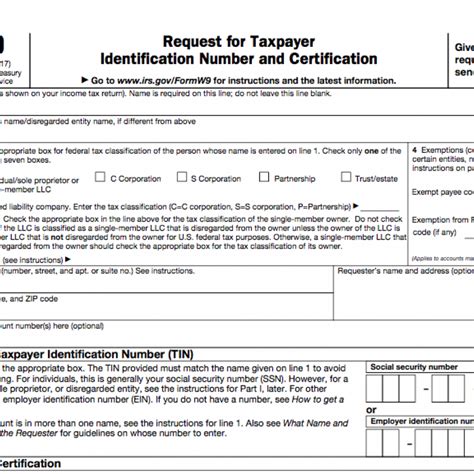
From a technical standpoint, the U6885 Payer ID must comply with the standards set forth by regulatory bodies and industry organizations. This includes adherence to EDI standards such as ANSI X12 and NCPDP for pharmacy claims. Compliance with these standards ensures that the electronic transmission of claims and payment information is secure, efficient, and consistent across different payers and providers. Furthermore, the use of standardized identifiers like the U6885 Payer ID supports the interoperability of healthcare data, facilitating the exchange of information between different entities in the healthcare system.
Evidence-Based Analysis
Studies and industry reports have highlighted the benefits of using standardized identifiers like the U6885 Payer ID in electronic claims processing. These benefits include reduced claim rejection rates, faster payment cycles, and improved provider satisfaction. For instance, a study by the Centers for Medicare and Medicaid Services (CMS) found that the implementation of standardized electronic claims submission processes, including the use of unique payer identifiers, resulted in significant reductions in claim processing times and errors. Similarly, an analysis by a leading healthcare consulting firm demonstrated that providers who regularly update and verify their payer IDs experience fewer payment delays and denials compared to those who do not.
What is the purpose of the U6885 Payer ID in healthcare claims processing?
+The U6885 Payer ID is used to identify the payer to whom the claim is being submitted, ensuring that claims are directed to the correct payer for timely and accurate payment processing.
How does the U6885 Payer ID contribute to the efficiency of the healthcare revenue cycle?
+The U6885 Payer ID helps streamline the revenue cycle by reducing errors in claims submission, facilitating timely payment, and automating the payment process through electronic remittance advice (ERA) and electronic funds transfer (EFT).
What are the consequences of not regularly updating the U6885 Payer ID?
+Failing to update the U6885 Payer ID can lead to claim rejection, payment delays, and increased administrative burdens, ultimately affecting the financial performance and patient care capabilities of healthcare providers.
In conclusion, the U6885 Payer ID is a critical component of the healthcare claims processing system, ensuring that claims are accurately directed to payers and facilitating efficient payment processing. Its implementation and management require careful attention to technical specifications, compliance with industry standards, and ongoing maintenance to reflect changes in payer information. By understanding the role and importance of the U6885 Payer ID, healthcare providers and billing entities can optimize their revenue cycle management, reduce administrative costs, and improve patient care outcomes.