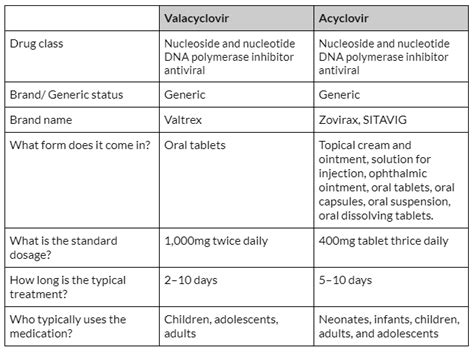
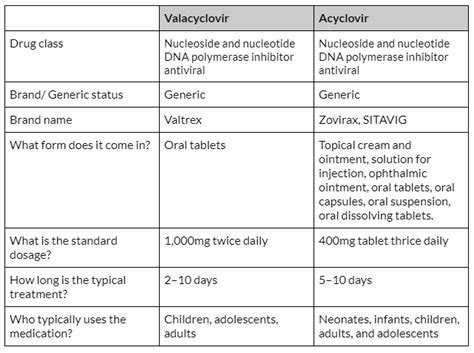
Valacyclovir and acyclovir are two antiviral medications that are commonly used to treat viral infections, particularly those caused by the herpes simplex virus (HSV) and varicella-zoster virus (VZV). While both medications are effective in managing these infections, there are key differences between them in terms of their mechanism of action, pharmacokinetics, and clinical applications. Understanding these differences is crucial for healthcare professionals to make informed decisions about which medication to prescribe for specific patient populations.
Key Points
- Valacyclovir is a prodrug of acyclovir, which means it is converted into acyclovir in the body.
- Valacyclovir has better oral bioavailability compared to acyclovir, leading to higher plasma concentrations.
- Both medications are effective against HSV and VZV, but valacyclovir may have a more favorable dosing regimen for certain patient groups.
- The side effect profiles of valacyclovir and acyclovir are similar, with gastrointestinal and neurological adverse effects being most common.
- The choice between valacyclovir and acyclovir depends on factors such as the severity of the infection, patient compliance, and potential drug interactions.
Pharmacological Properties

Valacyclovir is a prodrug of acyclovir, meaning that it is metabolized into acyclovir after administration. This conversion occurs via the enzyme valacyclovir hydrolase, which is predominantly found in the liver. The resulting acyclovir is then distributed throughout the body, where it exerts its antiviral effects by inhibiting viral DNA synthesis. Acyclovir, on the other hand, is available in its active form and does not require conversion. This difference in formulation affects their pharmacokinetic profiles, with valacyclovir demonstrating approximately 55% oral bioavailability compared to acyclovir’s 15-20%. This higher bioavailability of valacyclovir translates into higher plasma concentrations of acyclovir when valacyclovir is administered, potentially leading to improved efficacy in certain clinical scenarios.
Antiviral Spectrum and Efficacy
Both valacyclovir and acyclovir are effective against a range of viral infections, including genital herpes (HSV-2), cold sores (HSV-1), and shingles (VZV). They work by selectively inhibiting the replication of these viruses, thereby reducing the severity and duration of symptoms. Clinical trials have demonstrated that valacyclovir and acyclovir have comparable efficacy in the treatment of these conditions, with valacyclovir offering the advantage of less frequent dosing due to its higher bioavailability. For example, valacyclovir can be administered twice daily for the treatment of genital herpes, whereas acyclovir may require more frequent dosing, typically three to five times a day.
| Medication | Oral Bioavailability | Dosing Frequency |
|---|---|---|
| Valacyclovir | 55% | Twice daily |
| Acyclovir | 15-20% | Three to five times daily |
Clinical Applications and Safety Profile
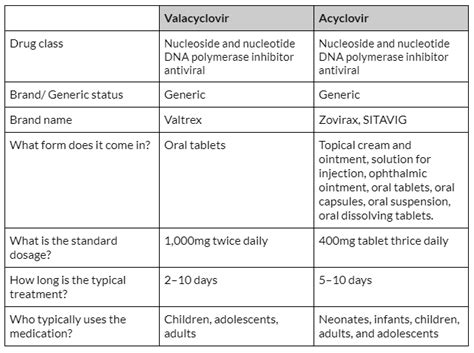
The safety profiles of valacyclovir and acyclovir are generally similar, with both medications being well-tolerated in the majority of patients. Common adverse effects include nausea, vomiting, diarrhea, and headache. Neurological adverse effects, such as dizziness and confusion, can occur but are less common. It is essential to monitor renal function in patients taking these medications, especially in those with pre-existing renal impairment, as both valacyclovir and acyclovir are excreted by the kidneys. The potential for drug interactions should also be considered, particularly with medications that affect renal function or share similar side effect profiles.
Special Considerations
In certain patient populations, such as the elderly or those with compromised immune systems, the choice between valacyclovir and acyclovir may need to be made with caution. For example, elderly patients may have reduced renal function, necessitating dose adjustments to prevent accumulation of the drug and potential toxicity. Similarly, immunocompromised patients may require higher doses or more prolonged treatment durations to effectively manage viral infections, which could impact the choice between valacyclovir and acyclovir based on their pharmacokinetic profiles and the specific clinical scenario.
What is the primary difference between valacyclovir and acyclovir?
+Valacyclovir is a prodrug that is converted into acyclovir in the body, offering higher oral bioavailability and potentially more convenient dosing regimens.
Are valacyclovir and acyclovir equally effective against viral infections?
+Yes, both medications are effective against HSV and VZV infections, but their efficacy can vary depending on the specific clinical scenario, patient compliance, and dosing regimen.
What factors influence the choice between valacyclovir and acyclovir?
+The choice between valacyclovir and acyclovir depends on factors such as the severity of the infection, potential drug interactions, patient compliance, and renal function.
In conclusion, valacyclovir and acyclovir are valuable antiviral medications used in the management of HSV and VZV infections. While they share a common mechanism of action, their differences in pharmacokinetics, dosing regimens, and clinical applications make one more suitable than the other in specific patient populations. Healthcare professionals must consider these factors, along with the individual patient’s needs and medical history, to make informed decisions about which medication to prescribe. As research continues to evolve, understanding the nuances of these antiviral agents will remain crucial in optimizing treatment outcomes for patients with viral infections.