The process of disinfecting medical equipment is a critical aspect of preventing the spread of infections and ensuring patient safety in healthcare settings. Among the various methods employed for disinfection, the use of heat and alcohol are two of the most common and effective approaches. Heat, in the form of autoclaving or dry heat sterilization, is widely recognized for its ability to kill a broad spectrum of microorganisms, including bacteria, viruses, and fungi. On the other hand, alcohol, typically ethanol or isopropanol, is used for surface disinfection due to its rapid action against many types of microorganisms.
The efficacy of heat in disinfecting medical equipment can be attributed to its denaturing effect on proteins, which are essential for the structure and function of microbial cells. Autoclaving, which involves steam under pressure, is particularly effective because the high temperature (usually 121°C) and moisture work synergistically to destroy microorganisms. This method is suitable for heat-resistant equipment such as surgical instruments, gloves, and certain types of tubing. Dry heat sterilization, although less moist than autoclaving, also achieves high temperatures (usually 160°C to 170°C) that are lethal to microorganisms, but it requires longer exposure times compared to autoclaving.
Key Points
- Heat disinfection methods, including autoclaving and dry heat sterilization, are effective against a wide range of microorganisms.
- Alcohol is commonly used for surface disinfection due to its rapid action against many types of microorganisms.
- The choice between heat and alcohol disinfection depends on the type of medical equipment and its material compatibility.
- Proper protocols must be followed to ensure the effectiveness of disinfection and the safety of the equipment.
- Regular maintenance and quality control are crucial to prevent the spread of infections.
Alcohol Disinfection
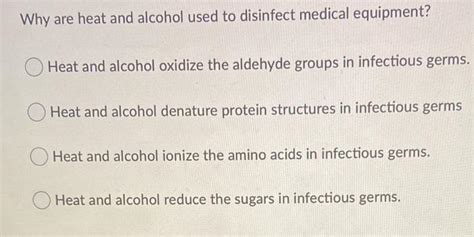
Alcohol disinfection is another critical method used in healthcare settings, particularly for surfaces and equipment that cannot withstand heat. Ethanol and isopropanol are the most commonly used alcohols for disinfection purposes. These alcohols work by denaturing proteins and disrupting cell membranes, leading to the death of microorganisms. The concentration of alcohol is crucial, with 70% ethanol and 70% isopropanol being the most effective concentrations for disinfection. Alcohol-based disinfectants are quick-acting and can be used on a variety of surfaces, but they may not be as effective against non-enveloped viruses and bacterial spores.
Limitations and Considerations
Despite their effectiveness, both heat and alcohol disinfection methods have their limitations and considerations. Heat disinfection is not suitable for all types of medical equipment, particularly those that are heat-sensitive or made from materials that can be damaged by high temperatures, such as plastics or electronics. Alcohol disinfection, while effective against many microorganisms, may not be suitable for all surfaces, especially those that are alcohol-sensitive, and it requires proper drying to prevent the growth of microorganisms in the moisture left behind.
| Disinfection Method | Effectiveness | Limitations |
|---|---|---|
| Autoclaving | High against bacteria, viruses, and fungi | Not suitable for heat-sensitive equipment |
| Dry Heat Sterilization | High against bacteria, viruses, and fungi | Longer exposure times required, not suitable for heat-sensitive equipment |
| Alcohol Disinfection | Effective against many microorganisms | May not be effective against non-enveloped viruses and bacterial spores, not suitable for alcohol-sensitive surfaces |

Best Practices for Disinfection

Implementing best practices for disinfection is crucial in healthcare settings to prevent the spread of infections. This includes selecting the appropriate disinfection method based on the type of equipment and the microorganisms to be targeted, following established protocols for disinfectant concentration and exposure time, ensuring that personnel are properly trained in disinfection procedures, and maintaining regular quality control measures to verify the effectiveness of disinfection practices.
Training and Quality Control
Training of healthcare personnel in proper disinfection techniques is essential to ensure that disinfection is carried out effectively. This includes understanding the principles of disinfection, the appropriate use of disinfectants, and the importance of following protocols. Regular quality control measures, such as microbial testing of disinfectants and monitoring of disinfection practices, are also critical to ensure that the disinfection processes in place are effective in reducing microbial loads to safe levels.
What is the most effective method for disinfecting heat-sensitive medical equipment?
+Alcohol disinfection is often the most effective method for heat-sensitive medical equipment, given its rapid action and suitability for a variety of surfaces. However, the choice of disinfectant should be based on the material compatibility of the equipment and the nature of the microorganisms to be targeted.
How often should disinfection protocols be reviewed and updated?
+Disinfection protocols should be reviewed and updated regularly, ideally every 6-12 months, or as needed based on changes in equipment, new microbial threats, or updates in disinfection guidelines from reputable health organizations.
What role does training play in ensuring effective disinfection practices?
+Training is crucial in ensuring that healthcare personnel understand the principles of disinfection, can select the appropriate disinfectant for the task, and follow established protocols correctly. Regular training sessions can help maintain high standards of disinfection practice and reduce the risk of infection transmission.
In conclusion, the disinfection of medical equipment using heat and alcohol are critical components of infection control strategies in healthcare settings. By understanding the principles, applications, and limitations of these methods, healthcare providers can make informed decisions about the best approaches for their specific needs. Continuous education, adherence to established protocols, and regular quality control measures are essential for maintaining effective disinfection practices and ensuring the safety of patients and healthcare workers.



