The concept of a Letter of Medical Necessity (LMN) is a crucial aspect of healthcare, particularly in the context of medical billing and insurance claims. It is a document that healthcare providers use to justify the medical necessity of a specific treatment, procedure, or service for a patient. The primary purpose of an LMN is to provide detailed information about a patient's medical condition, the recommended treatment, and the reasons why the treatment is necessary. This letter is typically required by insurance companies, Medicare, and Medicaid to determine the legitimacy of a claim and to ensure that the treatment is indeed medically necessary.
Understanding the Purpose of a Letter of Medical Necessity
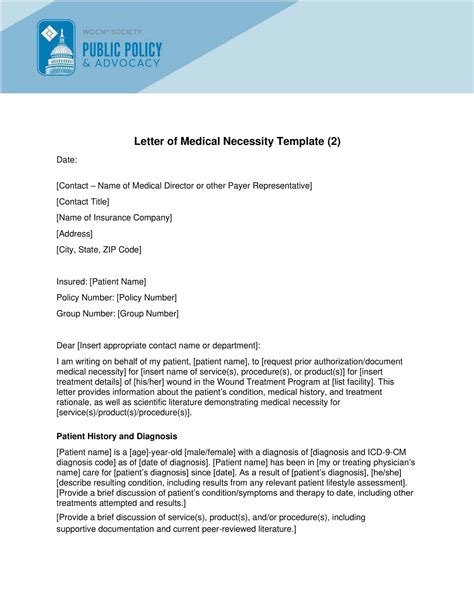
A Letter of Medical Necessity serves as a formal declaration from a healthcare provider, explaining the medical rationale behind a particular treatment or service. It outlines the patient’s diagnosis, the treatment plan, and the expected outcomes. The letter must be written in a clear and concise manner, using medical terminology and including all relevant details about the patient’s condition and the proposed treatment. The goal is to convince the insurance company or payer that the treatment is not only necessary but also the most appropriate option for the patient’s specific circumstances.
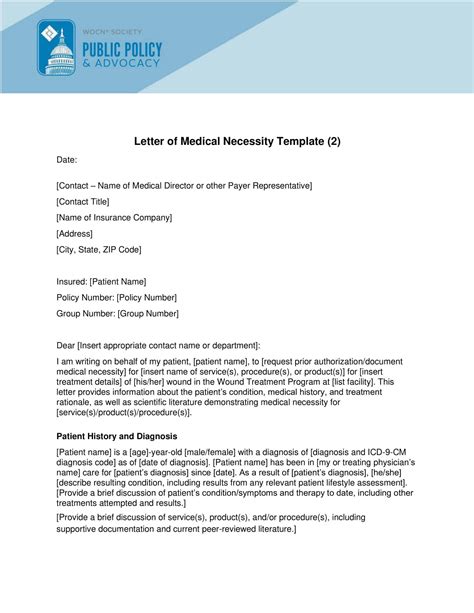
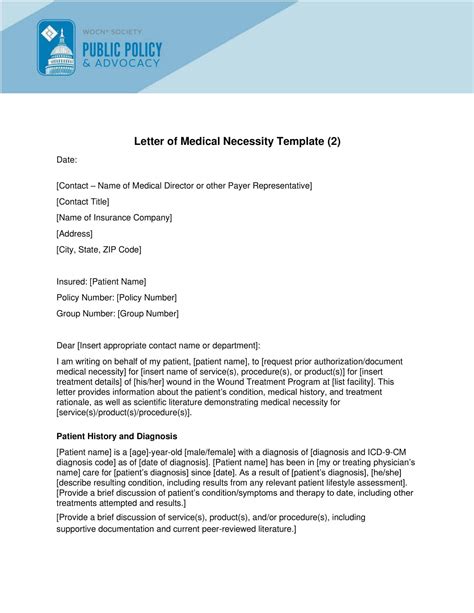
Key Components of a Letter of Medical Necessity
A comprehensive LMN should include several key components to effectively communicate the medical necessity of the treatment. These components include:
- Patient Information: Basic demographic information about the patient, including name, date of birth, and medical record number.
- Diagnosis: A clear statement of the patient’s diagnosis, including the ICD-10 code(s) relevant to the condition being treated.
- Treatment Description: A detailed description of the treatment, procedure, or service being recommended, including any relevant medical codes (e.g., CPT codes).
- Medical Rationale: An explanation of why the specific treatment is medically necessary for the patient, including how it will improve the patient’s condition or quality of life.
- Alternative Treatments Considered: A discussion of any alternative treatments that were considered and why they are not appropriate for the patient’s specific situation.
- Expected Outcomes: An outline of the expected outcomes of the treatment, including any potential risks or side effects.
| Component | Description |
|---|---|
| Patient Information | Basic demographic information |
| Diagnosis | Clear statement of the patient's diagnosis with ICD-10 codes |
| Treatment Description | Detail of the treatment with relevant medical codes |
| Medical Rationale | Explanation of why the treatment is medically necessary |
| Alternative Treatments | Discussion of considered alternatives |
| Expected Outcomes | Outline of expected outcomes and potential risks |
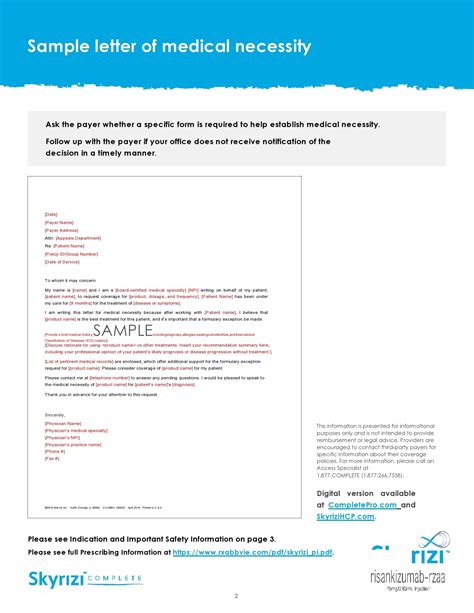
Best Practices for Writing a Letter of Medical Necessity
When writing a Letter of Medical Necessity, there are several best practices to keep in mind. First, it is essential to ensure that the letter is personalized to the patient’s specific situation, avoiding any generic templates that might not fully capture the nuances of the case. The letter should be written in a professional tone and must include all relevant medical information to support the claim. Additionally, it is crucial to proofread the letter carefully to avoid any errors or omissions that could delay the approval process.
Common Challenges and Solutions
Healthcare providers often face challenges when writing Letters of Medical Necessity, particularly in terms of ensuring that the letter is detailed enough to justify the treatment without being overly complex. One solution is to use a structured format that includes all the necessary components, while also allowing for the inclusion of specific details about the patient’s condition and treatment plan. Another challenge is the time-consuming nature of writing these letters, which can be mitigated by using software tools designed to streamline the process and reduce the administrative burden on healthcare providers.
Key Points
- A Letter of Medical Necessity is a critical document used to justify the medical necessity of a treatment or service.
- The letter must include the patient's diagnosis, treatment plan, and the medical rationale for the treatment.
- It is essential to write the letter in a clear and concise manner, using medical terminology and including all relevant details.
- Healthcare providers should ensure that the letter is personalized to the patient's specific situation and includes all necessary components.
- Using a structured format and software tools can help streamline the process and reduce administrative burdens.
In conclusion, a Letter of Medical Necessity is a vital tool in the healthcare system, serving as a bridge between healthcare providers and insurance companies to ensure that patients receive the necessary treatments. By understanding the purpose, components, and best practices for writing these letters, healthcare providers can navigate the complex process of medical billing and claims with greater ease, ultimately focusing on what matters most: delivering high-quality patient care.
What is the primary purpose of a Letter of Medical Necessity?
+The primary purpose of a Letter of Medical Necessity is to justify the medical necessity of a specific treatment, procedure, or service for a patient, providing detailed information about the patient’s medical condition and the recommended treatment.
What are the key components of a Letter of Medical Necessity?
+The key components include patient information, diagnosis, treatment description, medical rationale, alternative treatments considered, and expected outcomes.
Why is it important to personalize a Letter of Medical Necessity?
+Personalizing the letter ensures that it fully captures the nuances of the patient’s case, providing a clear and compelling justification for the treatment that is tailored to the patient’s specific needs and circumstances.