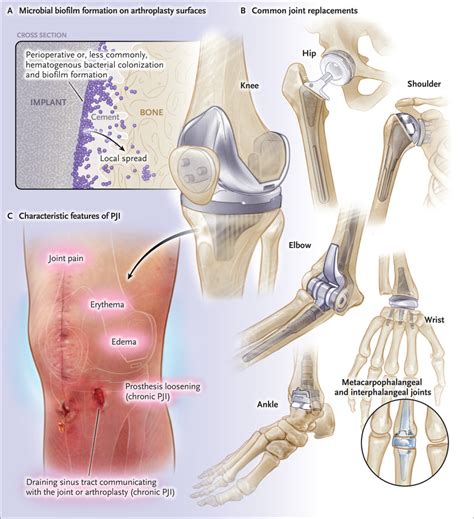
The medical field is replete with abbreviations, each serving a specific purpose in streamlining communication among healthcare professionals. One such abbreviation is "PJI," which stands for Prosthetic Joint Infection. Prosthetic joint infections are a severe complication that can arise following joint replacement surgery, where bacteria or other pathogens infect the prosthetic joint. This condition necessitates prompt diagnosis and treatment to prevent significant morbidity and potential mortality.
Understanding Prosthetic Joint Infections (PJIs)

PJI is a complex condition that requires a multidisciplinary approach for management. The diagnosis of PJI is based on a combination of clinical presentation, laboratory tests, and imaging studies. Patients with PJI may present with symptoms such as pain, swelling, redness, and warmth around the affected joint, along with systemic symptoms like fever. The diagnosis is often confirmed by the presence of pathogens in the synovial fluid or tissue surrounding the prosthetic joint, identified through cultures or molecular diagnostic techniques.
Risk Factors and Prevention Strategies
Risk factors for developing PJI include prior surgical site infections, compromised immune systems, diabetes, and a history of invasive procedures or infections. Preventing PJI is crucial and involves meticulous preoperative, perioperative, and postoperative care. This includes optimizing the patient’s health status before surgery, adhering to strict infection control practices during surgery, and monitoring for early signs of infection postoperatively. The use of prophylactic antibiotics and maintaining a sterile surgical environment are also critical in reducing the risk of PJI.
| Risk Factor | Prevention Strategy |
|---|---|
| Prior Infections | Preoperative screening and treatment |
| Immune Compromise | Optimizing immune status before surgery |
| Surgical Site Preparation | Adherence to infection control protocols |
Key Points
- PJI stands for Prosthetic Joint Infection, a serious complication of joint replacement surgery.
- Diagnosis involves clinical presentation, laboratory tests, and imaging studies.
- Risk factors include prior infections, immune compromise, and surgical site contamination.
- Prevention strategies focus on preoperative optimization, strict infection control, and postoperative monitoring.
- Treatment often involves a two-stage revision arthroplasty and antibiotic therapy.
The management and prevention of PJI are multifaceted, requiring a deep understanding of the underlying factors contributing to its development and the latest evidence-based practices for its treatment. By adopting a comprehensive approach that includes prevention strategies, early diagnosis, and effective treatment, healthcare professionals can significantly reduce the incidence and impact of PJI, improving patient outcomes and quality of life.
What are the common symptoms of Prosthetic Joint Infection?
+Common symptoms include pain, swelling, redness, and warmth around the affected joint, along with systemic symptoms like fever.
How is PJI diagnosed?
+Diagnosis is based on clinical presentation, laboratory tests (including cultures and molecular diagnostics), and imaging studies.
What is the typical treatment for PJI?
+Treatment often involves a two-stage revision arthroplasty, where the infected prosthetic is removed, followed by antibiotic therapy, and then re-implantation of a new prosthetic joint.
Meta Description: “PJI, or Prosthetic Joint Infection, is a serious complication of joint replacement surgery. Learn about its symptoms, diagnosis, risk factors, and treatment options to improve patient outcomes.” (151 characters)