The medical abbreviation "STSG" stands for Split-Thickness Skin Graft. It is a surgical procedure where a layer of skin is taken from a donor site on the patient's body and transplanted to a recipient site, typically to cover a wound or defect. The split-thickness skin graft is a popular method for wound closure due to its ease of harvest, minimal donor site morbidity, and ability to provide coverage for large surface areas.
Understanding the Procedure
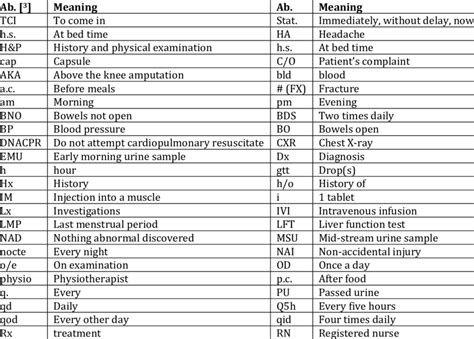
A split-thickness skin graft involves taking the top layers of skin, including the epidermis and a portion of the dermis, from a donor site. The graft is then secured to the recipient site using sutures, staples, or a dressing. The donor site is left to heal on its own, and the graft is allowed to integrate with the surrounding tissue at the recipient site. This procedure can be used for a variety of applications, including burn wounds, traumatic injuries, and surgical defects.
Advantages and Disadvantages
The STSG has several advantages, including its ability to provide coverage for large wounds, promote wound healing, and minimize donor site morbidity. However, it also has some disadvantages, such as the potential for graft failure, wound contraction, and the formation of hypertrophic scars. Additionally, the donor site may take several weeks to heal, and the graft may not match the surrounding skin in terms of color, texture, and thickness.
| Characteristics | Description |
|---|---|
| Donor Site | Typically the thigh, buttock, or abdominal area |
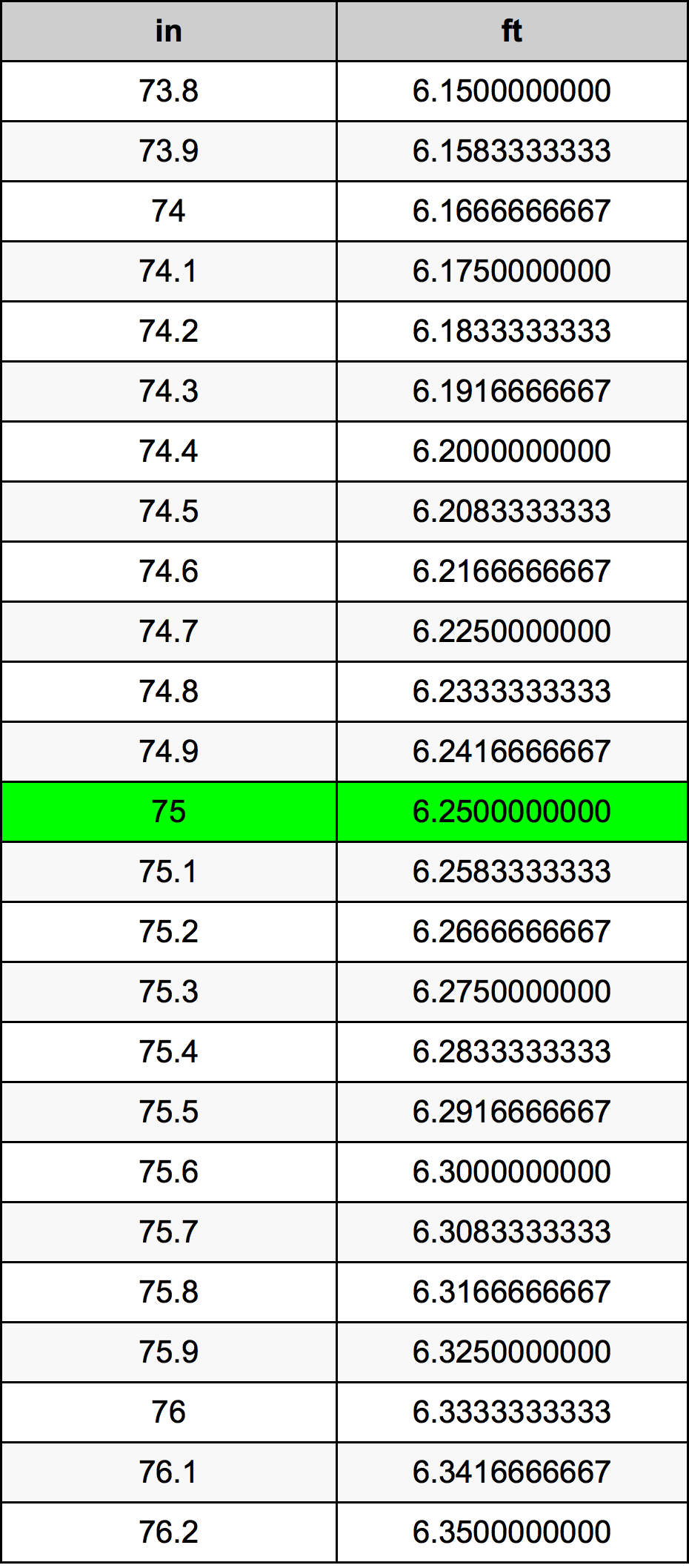
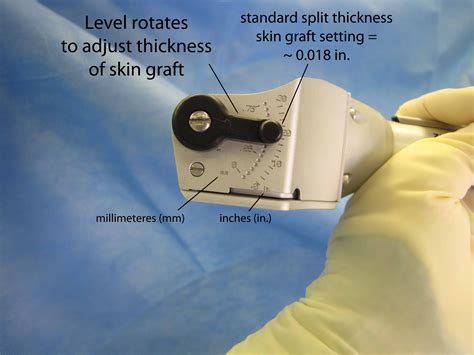
| Graft Thickness | 0.012-0.018 inches (0.3-0.45 mm) |
| Healing Time | 2-6 weeks for the donor site, 1-3 weeks for the graft |
| Complications | Graft failure, wound infection, hypertrophic scarring |
Indications and Contraindications
The STSG is indicated for a variety of conditions, including burns, traumatic injuries, and surgical defects. However, it may be contraindicated in patients with certain medical conditions, such as diabetes, peripheral vascular disease, or immunosuppression. The surgeon must carefully evaluate each patient to determine whether a STSG is the best treatment option.
Postoperative Care
After a STSG, the patient must follow a strict postoperative care regimen to ensure proper healing and minimize complications. This includes keeping the graft and donor site clean and dry, applying topical antibiotics, and avoiding strenuous activities. The patient must also attend follow-up appointments with the surgeon to monitor the healing process and address any concerns or complications that may arise.
Key Points
- The STSG is a surgical procedure that involves taking a layer of skin from a donor site and transplanting it to a recipient site.
- The procedure is commonly used to cover large wounds, promote wound healing, and minimize donor site morbidity.
- The STSG has several advantages, including its ability to provide coverage for large wounds and promote wound healing.
- However, it also has some disadvantages, such as the potential for graft failure and wound contraction.
- Proper wound preparation, meticulous graft harvesting, and careful postoperative care are essential for a successful STSG.
Future Directions
Research is ongoing to improve the outcomes of STSG and to develop new technologies and techniques for wound closure. This includes the use of bioengineered skin substitutes, wound dressings, and topical growth factors. Additionally, there is a growing interest in the use of minimally invasive procedures, such as endoscopic harvest of skin grafts, to reduce donor site morbidity and improve patient outcomes.
What is a split-thickness skin graft?
+A split-thickness skin graft is a surgical procedure that involves taking a layer of skin from a donor site and transplanting it to a recipient site to cover a wound or defect.
What are the advantages of a STSG?
+The advantages of a STSG include its ability to provide coverage for large wounds, promote wound healing, and minimize donor site morbidity.
What are the potential complications of a STSG?
+The potential complications of a STSG include graft failure, wound infection, and hypertrophic scarring.