The Medicaid freeze, a policy strategy employed by several states in the United States, has been a subject of intense debate and discussion among healthcare policymakers, economists, and social advocates. At its core, the Medicaid freeze refers to the practice of states pausing or halting the expansion of Medicaid, a joint federal-state program designed to provide health coverage to low-income individuals and families. This decision has profound implications for the healthcare landscape, affecting not only the lives of millions of Americans but also the financial and operational dynamics of healthcare systems across the country.
Key Points
- The Medicaid freeze affects low-income individuals and families, potentially leaving them without access to essential healthcare services.
- States that implement a Medicaid freeze may face significant financial and operational challenges in their healthcare systems.
- The policy has been influenced by various factors, including political ideologies, economic considerations, and the evolution of healthcare policy at the federal level.
- Advocates of Medicaid expansion argue that it improves health outcomes, reduces mortality rates, and has positive economic impacts on local communities.
- Opponents of expansion often cite concerns about increased state expenditures, potential inefficiencies in the program, and philosophical objections to government-provided healthcare.
Historical Context and Evolution of Medicaid

Medicaid was enacted in 1965 as part of the Social Security Act, with the aim of providing health insurance coverage to families with dependent children and individuals with disabilities who have limited income and resources. Over the years, the program has undergone numerous changes, with one of the most significant reforms being the Affordable Care Act (ACA) of 2010. The ACA allowed states to expand Medicaid eligibility to include adults with incomes up to 138% of the federal poverty level, with the federal government covering a significant portion of the costs for the newly eligible population.
Implications of the Medicaid Freeze
The decision to freeze Medicaid expansion has multifaceted implications. On one hand, it can lead to a reduction in the number of uninsured individuals, as those who would have been eligible for Medicaid under the expansion remain without coverage. This not only affects the health and wellbeing of these individuals but also has broader societal impacts, including increased healthcare costs due to untreated conditions and a higher likelihood of medical bankruptcies. On the other hand, proponents of the freeze argue that it helps control state spending and avoids the potential for increased taxes or reallocation of funds from other vital public services.
| Category | Data |
|---|---|
| Number of Uninsured Individuals (Pre-ACA) | Approximately 47 million |
| Number of Uninsured Individuals (Post-ACA, 2020) | Around 27 million |
| Federal Funding for Medicaid Expansion | Initially 100%, phasing down to 90% by 2020 |

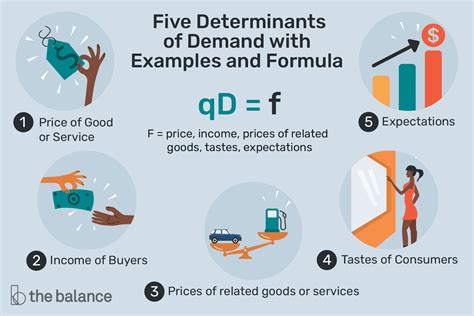
Economic and Social Impacts

The economic and social impacts of the Medicaid freeze are far-reaching. Economically, the expansion of Medicaid has been shown to generate jobs, stimulate local economies, and reduce the financial burden on hospitals and other healthcare providers who often absorb the costs of uncompensated care. Socially, Medicaid expansion has been associated with improved health outcomes, including better management of chronic diseases, reduced mortality rates, and enhanced overall quality of life for low-income individuals and families.
Forward-Looking Implications and Policy Considerations
As the healthcare landscape continues to evolve, policymakers must consider the forward-looking implications of the Medicaid freeze. This includes evaluating the potential effects on healthcare access, outcomes, and costs, as well as the broader economic and social impacts on communities. Policymakers must also navigate the complex interplay between federal and state policies, budgetary considerations, and the political will to address the pressing issues of healthcare access and affordability.
What are the primary reasons states implement a Medicaid freeze?
+States may implement a Medicaid freeze due to concerns about the financial burden of expansion, philosophical objections to government-provided healthcare, and the potential for inefficiencies within the Medicaid program.
How does the Medicaid freeze affect healthcare outcomes for low-income individuals and families?
+The Medicaid freeze can lead to reduced access to essential healthcare services, potentially resulting in poorer health outcomes, increased mortality rates, and a higher incidence of untreated medical conditions among affected populations.
What role does the federal government play in supporting Medicaid expansion?
+The federal government provides significant financial support for Medicaid expansion, covering at least 90% of the costs for the newly eligible population. This funding is crucial for states considering expansion, as it helps mitigate the financial burden and ensures that more individuals have access to healthcare.
In conclusion, the Medicaid freeze is a complex policy issue with significant implications for healthcare access, outcomes, and the broader economic and social fabric of communities. As policymakers and stakeholders navigate this critical issue, it’s essential to consider the multifaceted impacts of the Medicaid freeze, weighing the potential benefits and drawbacks while striving to ensure that all individuals, regardless of income or social status, have access to the healthcare services they need to thrive.