Lewy body dementia (LBD) is a progressive neurodegenerative disorder characterized by the presence of abnormal protein clumps called Lewy bodies in the brain. It is the second most common form of dementia after Alzheimer's disease, affecting approximately 1.4 million people in the United States. The symptoms of LBD can vary widely, but they often include cognitive decline, visual hallucinations, sleep disturbances, and motor dysfunction similar to Parkinson's disease. Managing LBD requires a comprehensive approach, including medication, to alleviate symptoms and improve the quality of life for patients and their caregivers.
Key Points
- Lewy body dementia is a progressive neurodegenerative disorder with no cure, but symptoms can be managed with medication and other interventions.
- Cholinesterase inhibitors are the primary medications used to treat cognitive symptoms in LBD.
- Antipsychotics are used with caution to manage hallucinations and delusions due to their potential to worsen motor symptoms.
- Levodopa and other dopaminergic agents can be used to manage parkinsonian motor symptoms but may exacerbate hallucinations.
- Non-pharmacological approaches, including behavioral interventions and support for caregivers, are crucial components of LBD management.
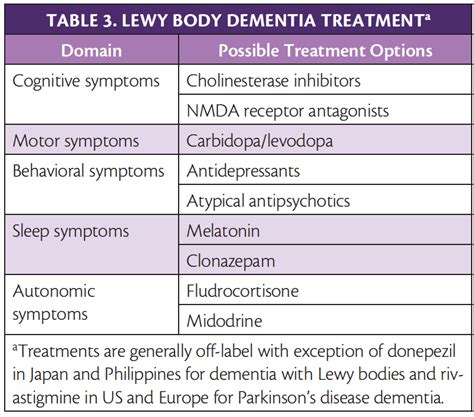
Medications for Cognitive Symptoms
Cognitive symptoms in LBD, such as memory loss, confusion, and difficulty with thinking and reasoning, can be challenging to manage. Cholinesterase inhibitors, such as rivastigmine, galantamine, and donepezil, are the primary medications used to treat these symptoms. These drugs work by increasing the levels of acetylcholine in the brain, a neurotransmitter that is involved in memory and learning. Studies have shown that cholinesterase inhibitors can improve cognitive function and behavioral symptoms in patients with LBD, although the effectiveness can vary among individuals.
Cholinesterase Inhibitors
Rivastigmine is often considered a first-line treatment for cognitive symptoms in LBD due to its dual inhibition of acetylcholinesterase and butyrylcholinesterase, which may provide additional benefits. Galantamine and donepezil are also effective, with donepezil being one of the most commonly used due to its once-daily dosing and well-established safety profile. The choice of cholinesterase inhibitor depends on the patient’s specific needs, side effect profile, and response to treatment.
| Medication | Primary Use | Common Side Effects |
|---|---|---|
| Rivastigmine | Cognitive symptoms in LBD | Nausea, vomiting, diarrhea, fatigue |
| Galantamine | Cognitive symptoms in LBD | Nausea, vomiting, diarrhea, dizziness |
| Donepezil | Cognitive symptoms in LBD and Alzheimer's disease | Nausea, diarrhea, insomnia, muscle cramps |

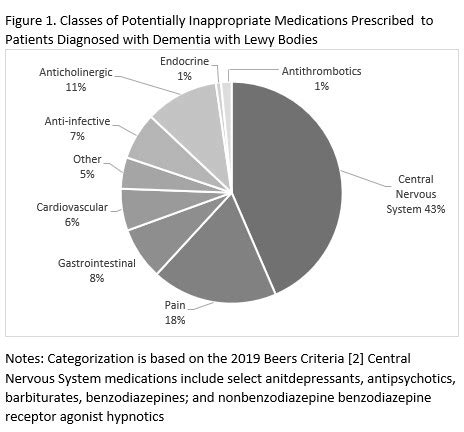
Management of Hallucinations and Delusions
Hallucinations and delusions are common in LBD and can be distressing for both patients and caregivers. Antipsychotic medications are sometimes used to manage these symptoms, but they must be used with caution due to the risk of worsening motor symptoms, a condition known as neuroleptic malignant syndrome. Quetiapine and clozapine are among the antipsychotics that have been used off-label for this purpose, although their effectiveness and safety in LBD are not well established.
Approach to Antipsychotic Use
The decision to use antipsychotics in LBD should be made on a case-by-case basis, considering the severity of symptoms and the potential risks. Non-pharmacological interventions, such as behavioral therapy and environmental modifications, should always be the first line of treatment for hallucinations and delusions. When antipsychotics are deemed necessary, they should be initiated at low doses and titrated slowly to minimize side effects.
Motor Symptoms Management
Patients with LBD often experience motor symptoms similar to those seen in Parkinson’s disease, such as tremors, stiffness, and bradykinesia (slow movement). Levodopa, in combination with carbidopa, is the most effective treatment for these symptoms but can sometimes exacerbate hallucinations. Other dopaminergic agents, like pramipexole and ropinirole, may also be used, although their efficacy in LBD is less well established than in Parkinson’s disease.
Considerations for Motor Symptom Treatment
Treating motor symptoms in LBD requires a delicate balance to avoid exacerbating other symptoms, particularly hallucinations. The dosage and type of medication should be carefully selected and monitored. In some cases, the benefits of treating motor symptoms may outweigh the risks, especially if the symptoms significantly impact the patient’s quality of life.
What are the most common medications used to treat Lewy body dementia?
+Cholinesterase inhibitors, such as rivastigmine, galantamine, and donepezil, are primarily used to treat cognitive symptoms. For motor symptoms, levodopa and other dopaminergic agents may be used, and antipsychotics like quetiapine are used cautiously for hallucinations and delusions.
How are hallucinations and delusions managed in LBD?
+Hallucinations and delusions are first managed with non-pharmacological interventions. If necessary, antipsychotics are used with caution due to the risk of worsening motor symptoms. The choice of antipsychotic and the dosage are carefully considered to minimize risks.
What role do non-pharmacological interventions play in LBD management?
+Non-pharmacological interventions, including behavioral therapy, environmental modifications, and support for caregivers, are crucial in managing LBD. They can help reduce the severity of symptoms, improve the quality of life, and are often used in conjunction with medication.
In conclusion, managing Lewy body dementia requires a multifaceted approach that includes medication, non-pharmacological interventions, and support for patients and their caregivers. While there is no cure for LBD, understanding the role of different medications and interventions can help healthcare providers and families make informed decisions to improve the quality of life for those affected by this condition.